Berikut merupakan kutipan ilmiah kedokteran yang bermanfaat untuk diketahui sehingga disusun dan digunakan sebagai referensi pribadi. Semoga bermanfaat.
Perpustakaan Keluarga : Helmut Todo Tua Simamora dan dr. Olga Y.V Hutapea
Electrocardiography (ECG or EKG*) is the process of recording the electrical activity of the heart over a period of time using electrodes placed on a patient's body. These electrodes detect the tiny electrical changes on the skin that arise from the heart muscle depolarizing during each heartbeat.
In a conventional 12 lead ECG, ten electrodes are placed on the patient's limbs and on the surface of the chest. The overall magnitude of the heart's electrical potential is then measured from twelve different angles ("leads") and is recorded over a period of time (usually 10 seconds). In this way, the overall magnitude and direction of the heart's electrical depolarization is captured at each moment throughout the cardiac cycle.[1] The graph of voltage versus timeproduced by this noninvasive medical procedure is referred to as an electrocardiogram (abbreviated ECG or EKG).
During each heartbeat, a healthy heart will have an orderly progression of depolarization that starts with pacemaker cells in the sinoatrial node, spreads out through the atrium, passes through the atrioventricular node down into thebundle of His and into the Purkinje fibers spreading down and to the left throughout the ventricles. This orderly pattern of depolarization gives rise to the characteristic ECG tracing. To the trained clinician, an ECG conveys a large amount of information about the structure of the heart and the function of its electrical conduction system.[2] Among other things, an ECG can be used to measure the rate and rhythm of heartbeats, the size and position of the heart chambers, the presence of any damage to the heart's muscle cells or conduction system, the effects of cardiac drugs, and the function of implanted pacemakers.[3]

| Electrocardiography | |
|---|---|
| Intervention | |

ECG of a heart in normal sinus rhythm.
| |
| ICD-9-CM | 89.52 |
| MeSH | D004562 |
| MedlinePlus | 003868 |
History
The etymology of the word is derived from the Greek electro, because it is related to electrical activity, kardio, Greek for heart, and graph, a Greek root meaning "to write".
Alexander Muirhead is reported to have attached wires to a feverish patient's wrist to obtain a record of the patient's heartbeat in 1872 at St Bartholomew's Hospital.[4] Another early pioneer was Augustus Waller, of St Mary's Hospital inLondon.[5] His electrocardiograph machine consisted of a Lippmann capillary electrometer fixed to a projector. The trace from the heartbeat was projected onto a photographic plate that was itself fixed to a toy train. This allowed a heartbeat to be recorded in real time.
An initial breakthrough came when Willem Einthoven, working in Leiden, the Netherlands, used the string galvanometer he invented in 1901.[6] This device was much more sensitive than both the capillary electrometer Waller used and the string galvanometer that had been invented separately in 1897 by the French engineer Clément Ader.[7] Einthoven assigned the letters P, Q, R, S, and T to the various deflections,[8] and described the electrocardiographic features of a number of cardiovascular disorders. In 1924, he was awarded the Nobel Prize in Medicine for his discovery.[9]
Though the basic principles of that era are still in use today, many advances in electrocardiography have been made over the years. Instrumentation has evolved from a cumbersome laboratory apparatus to compact electronic systems that often include computerized interpretation of the electrocardiogram.[10]
Medical uses
Reasons for performing electrocardiography include:
- Suspected heart attack
- Suspected pulmonary embolism
- A third heart sound, fourth heart sound, a cardiac murmur[11] or other findings to suggest structural heart disease
- Perceived cardiac dysrhythmias[11]
- Fainting or collapse[11]
- Seizures[11]
- Monitoring the effects of a heart medication
- Assessing severity of electrolyte abnormalities, such as hyperkalemia
The United States Preventive Services Task Force does not recommend electrocardiography for routine screening procedure in patients without symptoms and those at low risk for coronary heart disease.[12][13] This is because an ECG may falsely indicate the existence of a problem, leading to misdiagnosis, the recommendation of invasive procedures, or overtreatment. However, persons employed in certain critical occupations, such as aircraft pilots,[14] may be required to have an ECG as part of their routine health evaluations.
Continuous ECG monitoring is used to monitor critically ill patients, patients undergoing general anesthesia,[11] and patients who have an infrequently occurring cardiac dysrhythmia that would be unlikely be seen on a conventional ten second ECG.
Interpretation[edit]
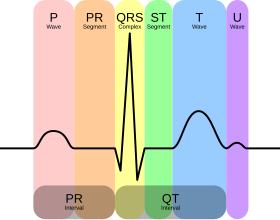
A typical ECG tracing is a repeating cycle of three electrical entities: a P wave (atrial depolarization), a QRS complex (ventricular depolarization) and a T wave (ventricular repolarization). The ECG is traditionally interpreted methodically in order to not miss any important findings.
Rate and rhythm[edit]
A heart rate between 60 and 100 beats per minute is considered normal. A heart rate slower than 60 beats per minute is said to be bradycardic and a rate faster than 100 beats per minute is said to be tachycardic. The physiologic rhythm of the heart is normal sinus rhythm, wherein the sinoatrial node initiates the cardiac cycle. In normal sinus rhythm a p-wave precedes every QRS complex and the rhythm is generally regular. If this is not the case, the patient may have a cardiac arrhythmia.
There are different types of rhythms that can cause the heart rate to be too fast or too slow. Many athletes can have a normal resting heart rate of less than 60 beats a minute. The key indicator of whether a slow heart rate is a problem is whether the person is having any kind of symptoms. One of the primary rhythms that can cause the heart rate to be slow and symptomatic is known as aheart block. There are many types of heart block, but the most common is an AV block.
There are also many rhythms that can cause the heart rate to be fast, the most common of which is sinus tachycardia. In sinus tachycardia, the depolarization is still starting in the normal pacemaker of the heart, called the Sino-Atrial or SA node. When the heart rhythm is no longer initiated in the SA node but is also initiating in various atrial foci then the heart rate can become irregular and can develop into atrial fibrillation (A-fib) or atrial flutter. A-fib can become unstable when the heart rate is above 100. The risk of rapid A-fib is that the heart is not beating efficiently and the blood that is pooling in the atria of the heart can begin to clot, putting the person at a high risk of stroke or heart attack. This is the reason many people with A-fib have to take blood thinners for the rest of their life. Other fast rhythms include supraventricular tachycardia, ventricular fibrillation, and ventricular tachycardia.[15] The heart rate can be approximated quickly by dividing 300 by the number of large boxes between two consecutive QRS complexes on the EKG paper.
Axis
The heart's electrical axis is the general direction of the ventricular depolarization wavefront (or mean electrical vector) in the frontal plane (the plane of the limb leads and augmented limb leads). The QRS axis can be determined by looking for the limb lead or augmented limb lead with the greatest positive amplitude of its R wave. A lead can only detect changes in voltage that are aligned with that lead; therefore the lead that is best aligned with the axis of ventricular depolarization will have the tallest positive QRS complex.
The normal QRS axis is generally down and to the left, following the anatomical orientation of the heart within the chest. An abnormal axis suggests a change in the physical shape and orientation of the heart, or a defect in its conduction system that causes the ventricles to depolarize in an abnormal way.
| Normal | −30° to 90° | Normal |
| Left axis deviation | −30° to −90° | May indicate left ventricular hypertrophy, left anterior fascicular block, or an old inferior q-wave myocardial infarction |
| Right axis deviation | +90° to +180° | May indicate right ventricular hypertrophy, left posterior fascicular block, or an old lateral q-wave myocardial infarction |
| Indeterminate axis | +180° to −90° | Rarely seen; considered an 'electrical no-man's land' |
A normal axis can be quickly identified if the QRS complexes in leads I and aVF are both upright. Lead I is positioned at 0° and lead aVF is positioned at 90°. If the QRS is upright in both, its vector of depolarization must be somewhere between these two angles, and is therefore normal axis.
Amplitudes and intervals
All of the waves on an EKG tracing and the intervals between them have a predictable time duration, a range of acceptable amplitudes (voltages), and a typical morphology. Any deviation from the normal tracing is potentially pathological and therefore of clinical significance.
For ease of measuring the amplitudes and intervals, an EKG is printed on graph paper at a standard scale: each 1 mm (one small box on the standard EKG paper) represents 40 milliseconds of time on the x-axis, and 0.1 millivolts on the y-axis.

| Feature | Description | Pathology | Duration |
|---|---|---|---|
| P wave | The p-wave represents depolarization of the atria. Atrial depolarization spreads from the SA node towards the AV node, and from the right atrium to the left atrium. | The p-wave is typically upright in most leads except for aVR; an unusual p-wave axis (inverted in other leads) can indicate an ectopic atrial pacemaker. If the p wave is of unusually long duration, it may represent atrial enlargement. Typically a large right atrium gives a tall, peaked p-wave while a large left atrium gives a two-humped bifid p-wave. | <80 ms |
| PR interval | The PR interval is measured from the beginning of the P wave to the beginning of the QRS complex. This interval reflects the time the electrical impulse takes to travel from the sinus node through the AV node. | A PR interval shorter than 120 ms suggests that the electrical impulse is bypassing the AV node, as in Wolf-Parkinson-White syndrome. A PR interval consistently longer than 200 ms diagnoses first degree atrioventricular block. The PR segment (the portion of the tracing after the p-wave and before the QRS complex) is typically completely flat, but may be depressed inpericarditis. | 120 to 200 ms |
| QRS complex | The QRS complex represents the rapid depolarization of the right and left ventricles. The ventricles have a large muscle mass compared to the atria, so the QRS complex usually has a much larger amplitude than the P-wave. | If the QRS complex is wide (longer than 120 ms) it suggests disruption of the heart's conduction system, such as in LBBB, RBBB, or ventricular rhythms such asventricular tachycardia. Metabolic issues such as severehyperkalemia, or TCA overdose can also widen the QRS complex. An unusually tall QRS complex may representleft ventricular hypertrophy while a very low-amplitude QRS complex may represent a pericardial effusion orinfiltrative myocardial disease. | 80 to 100 ms |
| J-point | The J-point is the point at which the QRS complex finishes and the ST segment begins. | The J point may be elevated as a normal variant. The appearance of a separate J wave or Osborn wave at the J point is pathognomonic of hypothermia orhypercalcemia.[16] | |
| ST segment | The ST segment connects the QRS complex and the T wave; it represents the period when the ventricles are depolarized. | It is usually isoelectric, but may be depressed or elevated with myocardial infarction or ischemia. ST depression can also be caused by LVH or digoxin. ST elevation can also be caused by pericarditis, Brugada syndrome, or can be a normal variant (J-point elevation). | |
| T wave | The T wave represents the repolarization of the ventricles. It is generally upright in all leads except aVR and lead V1. | Inverted T waves can be a sign of myocardial ischemia,LVH, high intracranial pressure, or metabolic abnormalities. Peaked T waves can be a sign ofhyperkalemia or very early myocardial infarction. | 160 ms |
| Corrected QT interval(QTc) | The QT interval is measured from the beginning of the QRS complex to the end of the T wave. Acceptable ranges vary with heart rate, so it must be corrected to the QTc by dividing by the square root of the RR interval. | A prolonged QTc interval is a risk factor for ventricular tachyarrhythmias and sudden death. Long QT can arise as a genetic syndrome, or as a side effect of certain medications. An unusually short QTc can be seen in severe hypercalcemia. | <440 ms |
| U wave | The U wave is hypothesized to be caused by the repolarization of the interventricular septum. It normally has a low amplitude, and even more often is completely absent. | If the U wave is very prominent, suspect hypokalemia, hypercalcemia or hyperthyroidism.[17] |
Ischemia and infarction
Ischemia or non-ST elevation myocardial infarctions may manifest as ST depression or inversion of T waves.
ST elevation myocardial infarctions have different characteristic ECG findings based on the amount of time elapsed since the MI first occurred. The earliest sign ishyperacute T waves, peaked T-waves due to local hyperkalemia in ischemic myocardium. This then progresses over a period of minutes to elevations of the ST segment by at least 1 mm. Over a period of hours, a pathologic Q wave may appear and the T wave will invert. Over a period of days the ST elevation will resolve. Pathologic q waves generally will remain permanently.[18]
The coronary artery that has been occluded can be identified in an ST-elevation myocardial infarction based on the location of ST elevation. The LAD supplies the anterior wall of the heart, and therefore causes ST elevations in anterior leads (V1 and V2). The LCx supplies the lateral aspect of the heart and therefore causes ST elevations in lateral leads (I, aVL and V6). The RCA usually supplies the inferior aspect of the heart, and therefore causes ST elevations in inferior leads (II, III and aVF).
Artifacts
An EKG tracing is affected by patient motion. Some rhythmic motions (such as shivering or tremors) can create the illusion of cardiac dysrhythmia.[19] Artifacts are distorted signals caused by a secondary internal or external sources, such as muscle movement or interference from an electrical device.[20][21]
Distortion poses significant challenges to healthcare providers,[20] who employ various techniques[22] and strategies to safely recognize[23] these false signals.[medical citation needed] Accurately separating the ECG artifact from the true ECG signal can have a significant impact on patient outcomes and legal liabilities.[24][unreliable medical source?]
Electrodes and leads
Ten electrodes are used for a 12-lead ECG. The electrodes usually consist of a conducting gel, embedded in the middle of a self-adhesive pad. The most common type of electrodes for ECG application is silver/silver chloride.[26] The names and correct locations for each electrode are as follows:
| Electrode name | Electrode placement |
|---|---|
| RA | On the right arm, avoiding thick muscle. |
| LA | In the same location where RA was placed, but on the left arm. |
| RL | On the right leg, lateral calf muscle. |
| LL | In the same location where RL was placed, but on the left leg. |
| V1 | In the fourth intercostal space (between ribs 4 and 5) just to the right of the sternum (breastbone). |
| V2 | In the fourth intercostal space (between ribs 4 and 5) just to the left of the sternum. |
| V3 | Between leads V2 and V4. |
| V4 | In the fifth intercostal space (between ribs 5 and 6) in the mid-clavicular line. |
| V5 | Horizontally even with V4, in the left anterior axillary line. |
| V6 | Horizontally even with V4 and V5 in the midaxillary line. |
The term "lead" in electrocardiography refers to the 12 different vectors along which the heart's depolarization is measured and recorded. There are a total of six limb leads and augmented limb leads arranged like spokes of a wheel in the coronal plane (vertical) and six precordial leads that lie on the perpendicular transverse plane (horizontal). In medical settings, the term leads is also sometimes used to refer to the ten electrodes themselves, although this is not technically a correct usage of the term.
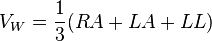
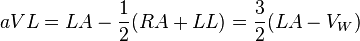
Each of these leads represents the electrical potential difference between two points. For each lead, the positive pole is one of the ten electrodes. In bipolar leads, the negative pole is a different one of the electrodes, while in unipolar leads, the negative pole is a composite pole known as Wilson's central terminal.[27] Wilson's central terminal VW is produced by averaging the measurements from the electrodes RA, LA, and LL to give an average potential across the body:
In a 12-lead ECG, all leads except the limb leads are unipolar (aVR, aVL, aVF, V1, V2, V3, V4, V5, and V6).
Limb leads
Leads I, II and III are called the limb leads. The electrodes that form these signals are located on the limbs—one on each arm and one on the left leg.[28][29][30] The limb leads form the points of what is known as Einthoven's triangle.[31]
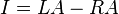
- Lead I is the voltage between the (positive) left arm (LA) electrode and right arm (RA) electrode:
- Lead II is the voltage between the (positive) left leg (LL) electrode and the right arm (RA) electrode:
- Lead III is the voltage between the (positive) left leg (LL) electrode and the left arm (LA) electrode:
Augmented limb leads
Leads aVR, aVL, and aVF are the augmented limb leads. They are derived from the same three electrodes as leads I, II, and III, but they use Goldberger's central terminal as their negative pole which is a combination of inputs from other two limb electrodes.
- Lead augmented vector right (aVR)' has the positive electrode on the right arm. The negative pole is a combination of the left arm electrode and the left leg electrode:
- Lead augmented vector left (aVL) has the positive electrode on the left arm. The negative pole is a combination of the right arm electrode and the left leg electrode:
- Lead augmented vector foot (aVF) has the positive electrode on the left leg. The negative pole is a combination of the right arm electrode and the left arm electrode:
Together with leads I, II, and III, augmented limb leads aVR, aVL, and aVF form the basis of the hexaxial reference system, which is used to calculate the heart's electrical axis in the frontal plane.
Precordial leads
The precordial leads lie in the transverse (horizontal) plane, perpendicular to the other six leads. The six precordial electrodes act as the positive poles for the six corresponding precordial leads: (V1, V2, V3, V4, V5 and V6). Wilson's central terminal is used as the negative pole.
Specialized leads
Additional electrodes may rarely be placed to generate other leads for specific diagnostic purposes. Right sided precordial leads may be used to better study pathology of the right ventricle. Posterior leads may be used to demonstrate the presence of a posterior myocardial infarction. A Lewis lead (requiring an electrode at the right sternal border in the second intercostal space) can be used to study pathological rhythms arising in the right atrium.
An esophogeal lead can be inserted to a part of the tract where the distance to the posterior wall of the left atrium is only approximately 5–6 mm (remaining constant in people of different age and weight).[32] An esophageal lead avails for a more accurate differentiation between certain cardiac arrhythmias, particularlyatrial flutter, AV nodal reentrant tachycardia and orthodromic atrioventricular reentrant tachycardia.[33] It can also evaluate the risk in people with Wolff-Parkinson-White syndrome, as well as terminate supraventricular tachycardia caused by re-entry.[33]
Lead locations on an ECG report
A standard 12-lead ECG report shows a 2.5 second tracing of each of the twelve leads. The tracings are most commonly arranged in a grid of four columns and three rows. the first column is the limb leads (I,II, and III), the second column is the augmented limb leads (aVR, aVL, and aVF), and the last two columns are the precordial leads (V1-V6).
Contiguity of leads
Each of the 12 ECG leads records the electrical activity of the heart from a different angle, and therefore align with different anatomical areas of the heart. Two leads that look at neighboring anatomical areas are said to becontiguous.
| Category | Leads | Activity |
|---|---|---|
| Inferior leads' | Leads II, III and aVF | Look at electrical activity from the vantage point of the inferior surface (diaphragmatic surface of heart) |
| Lateral leads | I, aVL, V5and V6 | Look at the electrical activity from the vantage point of the lateral wall of leftventricle |
| Septal leads | V1 and V2 | Look at electrical activity from the vantage point of the septal surface of the heart (interventricular septum) |
| Anterior leads | V3 and V4 | Look at electrical activity from the vantage point of the anterior wall of the right and left ventricles (Sternocostal surface of heart) |
In addition, any two precordial leads next to one another are considered to be contiguous. For example, though V4 is an anterior lead and V5 is a lateral lead, they are contiguous because they are next to one another.
The aging cardiovascular system undergoes many anatomic and physiologic changes. Increased vascular resistance, myocardial "stiffness," abnormalities of rhythmicity of the sinoatrial node, irregular cardiac rhythms, and alterations in heart rate and blood pressure responses are all seen more frequently in older patients. These changes are likely to impair these patients' ability to make the rapid adjustments necessary to maintain cardiac output during exercise and activity. When cardiovascular disease processes are superimposed on the "normal" concomitants of aging, greater alterations in hemodynamic response to exercise activity are noted than usually occur in younger cardiac patients. Exercise testing of older cardiac patients is safe and is usually needed to prescribe an appropriate intensity of exercise activity. The choice of the exercise protocol, the timing of the exercise test in relation to taking prescribed cardiac medication, the choice of exercise equipment, and special considerations for devices such as pacemakers and automatic implantable cardiodefibrillators must be considered before the exercise test is done. Many of these factors and the presence of either silent or overt cardiac symptoms or untoward hemodynamic events will also affect the exercise prescription. Elderly patients usually show substantial functional improvement when participating in a cardiac rehabilitation program and comply well with prescribed exercise. Early educational intervention may be crucial to reducing disability in these patients.
As can be expected from an organ responsible for getting blood throughout the body, the root of heart disease is when that blood flow is blocked.
Heart disease, or cardiovascular disease, encompasses a range of conditions, including blood vessel diseases such as coronary artery disease, problems with heart rhythm (arrhythmias) and congenital heart defects.
Symptoms and types
Coronary artery disease is the most common type of heart disease in the United States, according to the CDC. It occurs when cholesterol builds up in arteries — called plaque — narrowing the space blood can flow through, a condition called atherosclerosis.
In other words, "anything that blocks the vessel," said Lawrence Phillips, a cardiologist and assistant professor at NYU Langone Medical Center, in New York.
Ultimately, the narrowing can build up enough to cause chest pain and shortness of breath — called angina, or it can block the vessel completely, causing a heart attack. Heart attacks can also be caused by the rupture of a plaque that causes a blockage of the blood vessels, Phillips said. Over 1 million Americans suffer heart attacks each year, according to the American Heart Association.
Another cause of heart disease is an arrhythmia, a condition where the heart beats too quickly (tachycardia), too slowly (bradycardia) or irregularly. Symptoms can include a fluttering feeling in the chest, racing heartbeat, slow heartbeat, chest pain or discomfort, shortness of breath, lightheadedness, dizziness, fainting (syncope) or near fainting, according to the Mayo Clinic.
Heart disease may also be caused by problems a person is born with, known as congenital heart defects. Symptoms of heart defects in children can include pale gray or blue skin (cyanosis), swelling in the legs, abdomen or around the eyes, and shortness of breath during feeding in infants (causing poor weight gain), according to the Mayo Clinic.
Less serious congenital heart defects may not be diagnosed until late childhood or adulthood. These defects are not immediately life threatening, and symptoms include becoming short of breath or tired easily during exercise or activity, as well as swelling in the hands, ankles or feet.
Other forms of heart disease can be caused by weak heart muscle, heart infections, or diseases of the heart valves.
Diagnosis and tests
Five symptoms can indicate when someone is having a heart attack and requires immediate emergency care. These include pain in the jaw, neck or back; pain in the arms or shoulder; chest pain; lightheadedness or weakness; and shortness of breath, Phillips said.
Heart disease symptoms may differ for men and women, according to the Mayo Clinic. Men are more likely to have chest pain, while women are more likely to have shortness of breath, nausea and extreme fatigue.
A number of factors play a role in heart disease risk. Some include family history and age (if your relatives have heart disease or you are older, your risk goes up), but others you have more control over.
Much of the advice to avoid heart disease is the same health advice given for other conditions: stop smoking, exercise and eat a diet that is low in cholesterol and salt — cholesterol being the source of blockage and salt contributing to higher blood pressure. Other things to avoid in the diet include saturated fats, which typically come from animal fats and oils, and trans fats, which occur in vegetable oil, but have largely been removed from the marketplace because of consumer demand.
According to the NIH, diabetes can increase heart disease risk by as much as 100 percent, as the higher levels of glucose in the blood that are characteristic of diabetes can leave fatty deposits in blood vessels, which, like cholesterol plaques, can cause blockage of the heart.
Prevention
In addition to lifestyle changes, some treatments are available to help avoid heart disease. Many of these medications are designed to lower cholesterol.
There are two types of cholesterol. The first, LDL, is called “bad cholesterol” because it is the type that can build up and block blood vessels. The other, HDL, is called “good cholesterol” because it is responsible for transporting LDL to the liver, ultimately removing it from the blood stream.
Optimally, HDL cholesterol levels should be above 40 (measured in milligrams per deciliter of blood) and LDL cholesterol should be below 100, according to the CDC.
The FDA has approved a number of drugs for improving cholesterol levels. Perhaps the best-known are statins. They slow cholesterol production by the liver and speed up how fast it removed LDL cholesterol from the bloodstream.
Another class of drug to lower cholesterol is called bile acid sequestrants. These drugs remove bile acids from the body. Because the body produces these acids from LDL cholesterol, more LDL cholesterol will be broken down to replace them.
Niacin and fibrates are other drug classes for improving cholesterol levels. Both increase HDL cholesterol, and niacin lowers LDL cholesterol.
Treatment
Surgical options can also treat heart disease. Coronary angioplasty is performed over one million times each year on patients in the United States, according to the NIH. In this procedure, a balloon is threaded into the affected blood vessel and inflated, pushing the plaque blocking the artery to the sides of the vessel. Sometimes, this procedure is accompanied by placement of a stent — a mesh tube designed to hold the blood vessel open.
Despite all that is known about it, heart disease is the leading cause of death in both men and women in the United States, according to the CDC, claiming over 630,000 lives in 2006 — more than a quarter of all deaths.
The EKG (ECG) Waveform
EKG waveforms are displayed on monitors or paper. These EKG tracings have important features which can be analyzed to reveal a normal or an abnormal rhythm (a dysrrhythmia).
EKG can include various waveform components which are can be interpreted to understand if the EKG is a sinus rhythm or abnormal:
- P Wave
- PR Interval
- PR Segment
- QRS Complex
- QT Interval
- ST Segment
The P wave indicates atrial depolarization and it is normally an upward deflection in the EKG tracing. Next the QRS complex indicates ventricle repolarization. It typically starts with a negative deflection, then a large positive movement and then a negative movement, the S wave. A T wave normally follows the QRS complex. It is typically a upwards waveform, indicating repolarization of the ventricles. Intervals such as the PR interval, PR segment, QT interval and ST segment can also be analyzed to understand the heart's condition.
EKG Rhythm Types
The EKG Rhythms Self Test presents tracings grouped by type. You can uncheck any area that you have previously mastered.
Sinus Mechanisms
Atrial Rhythms
Junctional Rhythms
Ventricular Rhythms
Atrioventricular Blocks
Pacemaker Rhythms
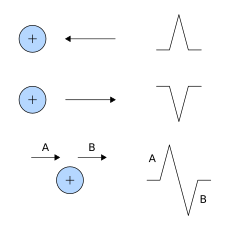
Bipolar recordings utilize standard limb lead configurations depicted at the right. By convention, lead I has the positive electrode on the left arm, and the negative electrode on the right arm, and therefore measures the potential difference between the two arms. In this and the other two limb leads, an electrode on the right leg serves as a reference electrode for recording purposes. In the lead II configuration, the positive electrode is on the left leg and the negative electrode is on the right arm. Lead III has the positive electrode on the left leg and the negative electrode on the left arm. These three bipolar limb leads roughly form an equilateral triangle (with the heart at the center) that is called Einthoven's triangle in honor of Willem Einthoven who developed the electrocardiogram in 1901. Whether the limb leads are attached to the end of the limb (wrists and ankles) or at the origin of the limb (shoulder or upper thigh) makes no difference in the recording because the limb can simply be viewed as a long wire conductor originating from a point on the trunk of the body.
Based upon universally accepted ECG rules, a wave a depolarization heading toward the left arm gives a positive deflection in lead I because the positive electrode is on the left arm. Maximal positive ECG deflection occurs in lead I when a wave of depolarization travels parallel to the axis between the right and left arms. If a wave of depolarization heads away from the left arm, the deflection is negative. Also by these rules, a wave of repolarization moving away from the left arm is recorded as a positive deflection. Similar statements can be made for leads II and III in which the positive electrode is located on the left leg. For example, a wave of depolarization traveling toward the left leg produces a positive deflection in both leads II and III because the positive electrode for both leads is on the left leg. A maximal positive deflection is recorded in lead II when the depolarization wave travels parallel to the axis between the right arm and left leg. Similarly, a maximal positive deflection is obtained in lead III when the depolarization wave travels parallel to the axis between the left arm and left leg.
If the three limbs of Einthoven's triangle (assumed to be equilateral) are broken apart, collapsed, and superimposed over the heart, then the positive electrode for lead I is said to be at zero degrees relative to the heart (along the horizontal axis) (see figure at right). Similarly, the positive electrode for lead II will be +60º relative to the heart, and the positive electrode for lead III will be +120º relative to the heart as shown to the right. This new construction of the electrical axis is called the axial reference system. With this system, a wave of depolarization traveling at +60º produces the greatest positive deflection in lead II. A wave of depolarization oriented +90º relative to the heart produces equally positive deflections in both lead II and III. In this latter example, lead I shows no net deflection because the wave of depolarization is heading perpendicular to the 0º, or lead I, axis (see ECG rules).
For a heart with a normal ECG and a mean electrical axis of +60º, the standard limb leads will appear as follows:
There are several methods for determining heart rate. Our first method is simple. Count the number of QRS complexes over a 6 second interval. Multiply by 10 to determine heart rate. This method works well for both regular and irregular rhythms. In the first image, we can count 7 QRS complexes, so the heart rate is 70.
The second method uses small boxes. Count the number of small boxes for a typical R-R interval. Divide this number into 1500 to determine heart rate. In the second image, the number of small boxes for the R-R interval is 21.5. The heart rate is 1500/21.5, which is 69.8.
In addition to the three bipolar limb leads described above, there are three augmented unipolar limb leads. These are termed unipolar leads because there is a single positive electrode that is referenced against a combination of the other limb electrodes. The positive electrodes for these augmented leads are located on the left arm (aVL), the right arm (aVR), and the left leg (aVF). In practice, these are the same electrodes used for leads I, II and III. (The ECG machine does the actual switching and rearranging of the electrode designations). The three augmented leads, along with the threestandard bipolar limb leads, are depicted as shown to the right using the axial reference system. The aVL lead is at -30° relative to the lead I axis; aVR is at -150° and aVF is at +90°. It is very important to learn which lead is associated with each axis.
The three augmented unipolar leads, coupled with the three bipolar leads, constitute the six limb leads of the ECG. These leads record electrical activity along a single plane, termed the frontal plane relative to the heart. Using the axial reference system and these six leads, it is simple to define the direction of an electrical vector at any given instant in time. If a wave of depolarization is spreading from right-to-left along the 0° axis, then lead I will show the greatest positive amplitude. If the direction of the electrical vector for depolarization is directed downwards (+90°), then aVF will show the greatest positive deflection. If a wave of depolarization is moving from left-to-right at +150°, then aVL will show the greatest negative deflection according to the rules for ECG interpretation.
For a heart with a normal ECG and mean electrical axis of +60°, the augmented leads will appear as shown below:
Sumber : Internet