Berikut merupakan kutipan ilmiah kedokteran yang sangat bermanfaat sehingga disusun dan digunakan sebagai referensi pribadi.
Perpustakaan keluarga :
Helmut Todo Tua Simamora dan dr. Olga Y.V Hutapea
Why Screening Tests Are Important
Remember that old saying, "An ounce of prevention is worth a pound of cure"? Getting checked early can help you stop diseases like cancer, diabetes, and osteoporosis in the very beginning, when they’re easier to treat. Screening tests can spot illnesses even before you have symptoms. Which screening tests you need depends on your age, family history, your own health history, and other risk factors.
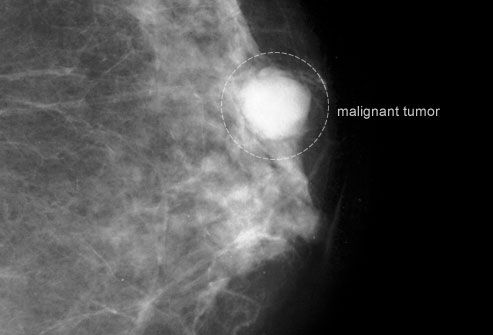
Breast Cancer
The earlier you find breast cancer, the better your chance of a cure. Small breast-cancers are less likely to spread to lymph nodes and vital organs like the lungs and brain. If you’re in your 20s or 30s, your health care provider should perform a breast exam as part of your regular check-up every one to three years. You may need more frequent screenings if you have any extra risk factors.
Screening With Mammography
Mammograms are low-dose X-rays that can often find a lump before you ever feel it, though normal results don’t completely rule out cancer. While you’re in your 40s, you should have a mammogram every year. Then between ages 50 and 74, switch to every other year. Of course, your doctor may recommend more frequent screenings if you’re at higher risk.
Cervical Cancer
With regular Pap smears, cervical cancer (pictured) is easy to prevent. The cervix is a narrow passageway between the uterus (where a baby grows) and the vagina (the birth canal). Pap smears find abnormal cells on the cervix, which can be removed before they ever turn into cancer. The main cause of cervical cancer is the human papillomavirus (HPV), a type of STD.
Screening for Cervical Cancer
During a Pap smear, your doctor scrapes some cells off your cervix and sends them to a lab for analysis. A common recommendation is that you should get your first Pap smear by age 21, and every two years after that. If you're 30 or older, you can get HPV tests, too, and wait a little longer between Pap smears. Both screenings are very effective in finding cervical cancer early enough to cure it.
Vaccines for Cervical Cancer
Two vaccines, Gardasil and Cervarix, can protect women under 26 from several strains of HPV. The vaccines don't protect against all the cancer-causing strains of HPV, however. So routine Pap smears are still important. What’s more, not all cervical cancers start with HPV.
Osteoporosis and Fractured Bones
Osteoporosis is a state when a person’s bones are weak and fragile. After menopause, women start to lose more bone mass, but men get osteoporosis, too. The first symptom is often a painful break after even a minor fall, blow, or sudden twist. In Americans age 50 and over, the disease contributes to about half the breaks in women and 1 in 4 among men. Fortunately, you can prevent and treat osteoporosis.
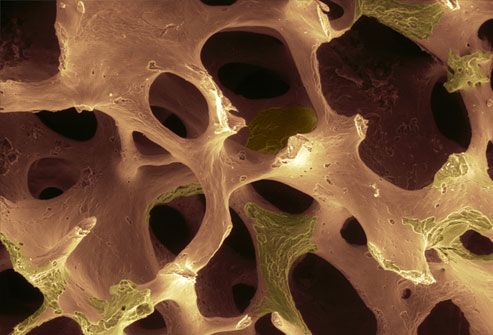
Osteoporosis Screening Tests
A special type of X-ray called dual energy X-ray absorptiometry (DXA) can measure bone strength and find osteoporosis before breaks happen. It can also help predict the risk of future breaks. This screening is recommended for all women age 65 and above. If you have risk factors for osteoporosis, you may need to start sooner.

Skin Cancer
There are several kinds of skin cancer, and early treatment can be effective for them all. The most dangerous is melanoma (shown here), which affects the cells that produce a person’s skin coloring. Sometimes people have an inherited risk for this type of cancer, which may increase with overexposure to the sun. Basal cell and squamous cell are common non-melanoma skin cancers.

Screening for Skin Cancer
Watch for any changes in your skin markings, including moles and freckles. Pay attention to changes in their shape, color, and size. You should also get your skin checked by a dermatologist or other health professional during your regular physicals.
High Blood Pressure
As you get older, your risk of high blood pressure increases, especially if you are overweight or have certain bad health habits. High blood pressure can cause life-threatening heart attacks or strokes without any warning. So working with your doctor to control it can save your life. Lowering your blood pressure can also prevent long-term dangers like heart disease and kidney failure.
Screening for High Blood Pressure
Blood pressure readings include two numbers. The first (systolic) is the pressure of your blood when your heart beats. The second (diastolic) is the pressure between beats. Normal adult blood pressure is below 120/80. High blood pressure, also called hypertension, is 140/90 or above. In between is prehypertension, a sort of early warning stage. Ask your doctor how often to have your blood pressure checked.
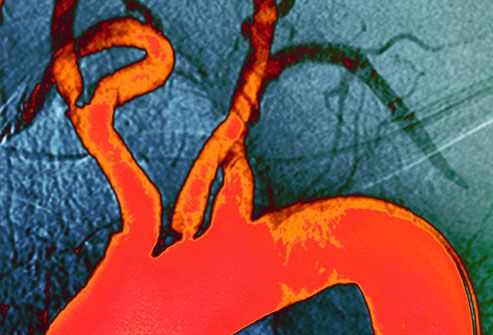
Cholesterol Levels
High cholesterol can cause plaque to clog your arteries (seen here in orange). Plaque can build up for many years without symptoms, eventually causing a heart attack or stroke. High blood pressure, diabetes, and smoking can all cause plaque to build up, too. It's a condition called hardening of the arteries or atherosclerosis. Lifestyle changes and medications can lower your risk.
Checking Your Cholesterol
To get your cholesterol checked, you’ll need to fast for 12 hours. Then you’ll take a blood test that measures total cholesterol, LDL "bad" cholesterol, HDL "good" cholesterol, and triglycerides (blood fat). If you’re 20 or older, you should get this test at least every five years.

Type 2 Diabetes
One-third of Americans with diabetes don’t know they have it. Diabetes can cause heart or kidney disease, stroke, blindness from damage to the blood vessels of the retina (shown here), and other serious problems. You can control diabetes with diet, exercise, weight loss, and medication, especially when you find it early. Type 2 diabetes is the most common form of the disease. Type 1 diabetes is usually diagnosed in children and young adults.
Screening for Diabetes
You’ll probably have to fast for eight hours or so before having your blood tested for diabetes. A blood sugar level of 100-125 may show prediabetes; 126 or higher may mean diabetes. Other tests include the A1C test and the oral glucose tolerance test. If you’re healthy and have a normal diabetes risk, you should be screened every three years starting at age 45. Talk to your doctor about getting tested earlier if you have a higher risk, like a family history of diabetes.

Human Immunodeficiency Virus (HIV)
HIV is the virus that causes AIDS. It’s spread through sharing blood or body fluids with an infected person, such as through unprotected sex or dirty needles. Pregnant women with HIV can pass the infection to their babies. There is still no cure or vaccine, but early treatment with anti-HIV medications can help the immune system fight the virus.
HIV Screening Tests
HIV can be symptom-free for many years. The only way to find out if you have the virus is with blood tests. The ELISA or EIA test looks for antibodies to HIV. If you get a positive result, you'll need a second test to confirm the results. Still, you can test negative even if you’re infected, so you may need to repeat the test. Everyone should get tested at least once between ages 13-64.
Preventing the Spread of HIV
Most newly infected people test positive around two months after being exposed to the virus. But in rare cases it may take up to six months to develop HIV antibodies. Use a condom during sex to avoid getting or passing on HIV or other STDs. If you have HIV and are pregnant, talk with your doctor about reducing the risk to your unborn child.

Colorectal Cancer
Colorectal cancer is the second most common cause of cancer death after lung cancer. Most colon cancers come from polyps (abnormal masses) that grow on the inner lining of the large intestine. The polyps may or may not be cancerous. If they are, the cancer can spread to other parts of the body. Removing polyps early, before they become cancerous, can prevent it completely.
Screening for Colorectal Cancer
A colonoscopy is a common screening test for colorectal cancer. While you’re mildly sedated, a doctor inserts a small flexible tube equipped with a camera into your colon. If she finds a polyp, she can often remove it right then. Another type of test is a flexible sigmoidoscopy, which looks into the lower part of the colon. If you’re at average risk, screening usually starts at age 50.

Glaucoma
Glaucoma happens when pressure builds up inside your eye. Without treatment, it can damage the optic nerve and cause blindness. Often, it produces no symptoms until your vision has already been damaged.
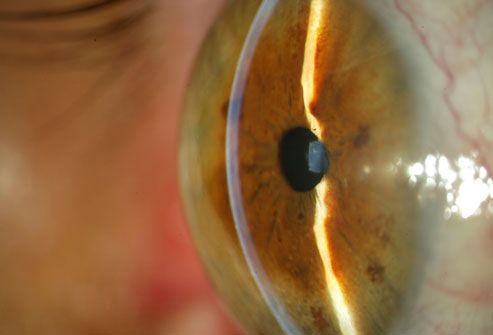
Glaucoma Screening
How often you should get your eyes checked depends on your age and risk factors. They include being African-American or Hispanic, being over 60, eye injury, steroid use, and a family history of glaucoma. People without risk factors or symptoms of eye disease should get a baseline eye exam, including a test for glaucoma, at age 40.
Ask Your Doctor About Screenings
It's good health sense to talk with your doctor about screening tests. Some tests, such as a Pap test or breast exam, should be a routine part of every woman’s health care. Other tests might be necessary based on your risk factors. Proper screening won’t always prevent a disease, but it can often find a disease early enough to give you the best chance of overcoming it.

Lung cancer accounts for over a fifth of cancer deaths
Lung cancer campaigners have called on health officials to warn people about the symptoms of the biggest cancer killer in Wales.
It accounts for more than a fifth of cancer deaths, more than bowel and breast cancer combined, according to a recent report from Public Health Wales.
The UK Lung Cancer Coalition said Wales also had one of the lowest survival rates in Europe for the disease.
The Welsh government accepted it had to go further in tackling lung cancer.
The call by a collection of charities, experts, professionals and healthcare companies follows a report on cancer in Wales from Public Health Wales in April which revealed lung cancer killed nearly 1,900 people in Wales in 2012 - 22% of the total number of deaths from cancer.
Lung cancer sufferers were also 12 times less likely to survive up to five years after diagnosis compared to people with breast cancer, according to the report.
Outcomes for lung cancer patients also remain poor in Wales when compared to other UK and European countries.
Dr Ian Lewis, director of research and policy at Cardiff-based cancer charity Tenovus, said: "More can be done to alert people to the signs and symptoms of this devastating disease in order to ensure earlier diagnosis and increase chances of survival."
"People don't like to bother their doctor and that's an issue for people not getting diagnosed early enough and not getting treatment.
"Prognosis overall for lung cancer is poor but if discovered early enough the success for treatment is improved greatly."
Mags Roberts, 58, from Cardiff, was diagnosed with lung cancer at the age of 52 after feeling breathless while walking up a hill in Pembrokeshire.
She said: "I was quite shocked as I'd never smoked so I never thought I'd get it.
"I wasn't ill in bed - I was going to work every day."
Mrs Roberts had to take early retirement from her job as a secondary school teacher for treatment with chemotherapy followed by courses of tablets which she continues to take to this day.
"I've got to live with it but I'm really fortunate to have a fantastic medical team looking after me and the support of my family and friends," said Mrs Roberts.
"It was only because I'd had asthma as a child that I thought of going to the doctor to check - it was lucky I went really.
"I'm really positive about life - I wake up every day and feel keen to make the most of it."
A Welsh government spokesperson said: "The Welsh NHS is spending more than ever on cancer care and while Wales has shown the biggest improvement in overall cancer survival rates of all UK nations, we need to go further when it comes to lung cancer.
"From this year all GPs will have to review every diagnosis of lung cancer to improve awareness and skills to support earlier diagnosis."
Dr Peter Bradley, executive director of public health development at Public Health Wales, said the organisation was already taking steps including anti-smoking campaigns.
He added: "We have also carried out a review of the way we support people to stay healthy, and invested in a wide ranging strategy to help us work towards a healthier, happier and fairer Wales."
General symptoms of lung cancer
- Having a cough most of the time
- A change in a cough you have had for a long time
- Being short of breath
- Coughing up phlegm (sputum) with signs of blood in it
- An ache or pain when breathing or coughing
- Loss of appetite
- Tiredness
- Losing weight

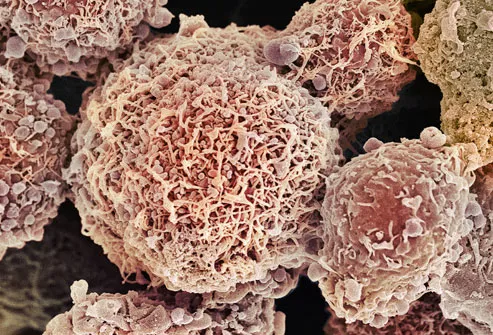
Leukaemia research may lead to new drugs for difficult-to-treat breast cancers, say scientists.
These types of tumours cannot be treated with the targeted drugs which have hugely improved survival.
A team in Glasgow says a faulty piece of DNA which causes leukaemia also has a role in some tumours and could help in research for new drugs.
Meanwhile, other researchers say they have taken tentative steps towards a blood test for breast cancer.
Oestrogen or progesterone positive breast cancers can be treated with hormone therapies such as Tamoxifen.
Another drug, Herceptin, works only on those tumours which are HER2-positive.
But around one in five breast cancers is "triple negative" meaning chemotherapy, radiotherapy or surgery are the only options.
Leukaemia
A team at the University of Glasgow investigated the role of the RUNX1 gene, which is one of the most commonly altered genes in leukaemia.
However, they have now shown it is also active in the most deadly of triple negative breast cancers.
Tests on 483 triple negative breast cancers showed patients testing positive for RUNX1 were four times more likely to die as a result of the cancer than those without it.
The results were published in the journal PLoS One.
One of the researchers, Dr Karen Blyth, said: "This opens up the exciting possibility of using it [RUNX1] as a new target for treatments."
She told the BBC: "First we need to prove this gene is causative to the cancer, if it is then what would happen if we did inhibit it?
"There's a couple of drugs in development in the US to target this gene from a leukaemia point of view, if they work we can test it in breast cancer cells."
.jpg)
Could leukaemia lead to insight into breast cancer?
However, the gene has a complex role. Normally it is vital for cell survival and plays a critical role in producing blood. However, depending on circumstances, it can either encourage or suppress tumours.
It means any use of a drug to target the gene might cause side-effects.
Dr Kat Arney, the science communications manager at Cancer Research UK, said: "There's still so much we need to understand about triple negative breast cancers, as they can be harder to treat in some people.
"Almost two out of three women with breast cancer now survive their disease beyond 20 years.
"But more must be done and we urgently need more studies like these, particularly in lesser-understood forms of the disease, to build on the progress we've already made and save more lives."
Blood test
In a separate development, scientists at University College London think they have taken the first steps towards a blood test for breast cancer.
They found changes in the DNA of immune cells in the blood of women who were at high risk of breast cancer as they had inherited the BRCA1 risk gene.
Prof Martin Widschwendter, from UCL said: "Surprisingly, we found the same signature in large cohorts of women without the BRCA1 mutation and it was able to predict breast cancer risk several years before diagnosis."
They think it could become the basis of a blood test.
Dr Matthew Lam, senior research officer at Breakthrough Breast Cancer, said: "These results are definitely promising and we're excited to learn how further research could build on these findings."
Sumber : Media online kesehatan








