Silahkan pilih dan klik angka yang Saudara inginkan .....
1
2
3
4
5
6
7
8
9
10
11
12
Rabu, 29 Januari 2014
BELAJAR TENTANG ATUR DIRI SENDIRI DAN PENYAKIT KENCING MANIS / GULA DARAH / DIABETES
Berikut merupakan kutipan ilmiah dari media online kesehatan yang sangat bermanfaat bagi Penulis yang disusun dan digunakan sebagai referensi pribadi.
Eat the Foods You Like
Having diabetes doesn't mean you can't eat your favorite foods. But you need to know how your food choices will affect your blood sugar. A diabetes educator or dietitian can help you learn skills -- such as counting carbs, reading food labels, and sizing up portions -- that will let you keep your diabetes in check while still enjoying your favorite meals.
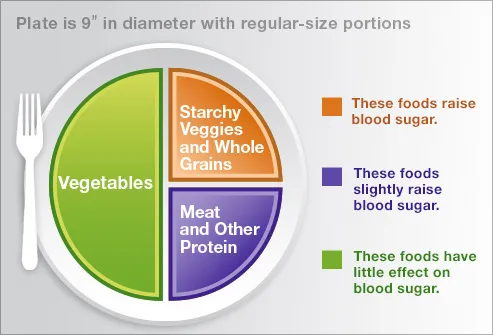
Define Your Plate
Use a rule of three to build a healthy, satisfying meal. This rule can help you lose weight and manage your diabetes by increasing your intake of non-starchy foods. Divide your plate in half. Fill one half with non-starchy vegetables like spinach or broccoli. Next, divide the empty side into two halves. Use one for starchy foods like bread or pasta. In the last section, add meat or another protein. You can also add an 8-ounce glass of low-fat milk and a ½ cup of fruit.
Write It Down
Get in the habit of writing down your critical information. Record your daily blood sugar levels to track how food, activity, and medicines affect your blood sugar and A1c test results. A written record can show you and your doctor whether your diabetes treatment is working over the long term. Writing down your goals and feelings in a journal may also help you stay on track and better communicate with your health care providers.
Have a Sick-Day Plan in Place
Common illnesses like colds, flu, and diarrhea can make your blood sugar rise. And having diabetes in turn may make it harder to fight off infections. Have a plan in case you get sick. Store snacks that are easy on the stomach but can still give you enough fluids and carbs. Check your blood sugar more often and know when to check for ketones and when to call your doctor. Get a flu shot every year.
Manage Your Medicine Cabinet
You may take pills or injections to manage your diabetes. Try to keep 3 days' worth of your diabetes medicines and supplies on hand in case of an emergency, as well as a list of all your medicines. Your drugs may interact with other medicines, even ones that can be bought without a prescription. Make sure to tell your doctor before you take any new medicine. And always take your list to your regular doctor and dental appointments.
Fight Everyday Stress With Activity
Living with diabetes can make you sad or unhappy at times. Stress not only affects your mood, but it can raise your blood sugar, too. Stress may cause you to make poor food choices and drink more alcohol. But an easy way to feel better from everyday stress is to get active. Being active raises the levels of chemicals in your brain that make you feel good. If you don't want to exercise in a gym, join a sports team or take dance lessons to keep moving.
Exercise in Short Sessions
It may be hard to find time to exercise. It can also be hard to keep going if you're not used to exercising for 30 minutes straight. The good news is you can spread your 30 minutes throughout the day. Three 10-minute walks are as good as 30 minutes at once. So don't hold out to exercise when you have a lot of time. Moderate physical activity (both strength building and cardio) will help you control your blood sugar, lower your blood pressure and cholesterol, and reduce stress.
Try Strength Workouts
All types of exercise can benefit people with diabetes. But training with weights or other resistance equipment may help you prevent muscle loss (lost muscle often leads to more fat). Several studies suggest strength training -- lifting weights, for example -- improves your reaction to insulin and your glucose tolerance. Of course, regular strength training can also improve your muscle mass and help you lose weight, too.
Check Your Feet Every Night
Use a hand mirror or ask someone to help you look for cuts, swelling, or color changes on your feet. Don't forget to look between your toes, too. If you see unhealed cuts or broken skin, call your doctor right away. Make foot care part of your daily routine: Wash and moisturize your feet and trim your toenails as needed. Talk to your doctor about treating corns or calluses. And have him examine your feet during every visit.
Choose a Date to Quit Smoking
If you smoke, picking a date to quit gives you the chance to prepare for it. You may need help beating the mental and physical parts of nicotine addiction. Stop-smoking programs, support groups, and wellness centers can offer professional help. Whether you quit cold turkey or use other treatments to help you quit, having time to prepare for it may improve your chances of success.
Drink Alcohol Only With Food
Your doctor may say it's OK for you to have an occasional drink. Drink alcohol only when you can eat something along with it, because alcohol can cause low blood sugar. Also have some water handy in case you get thirsty. Even so, mixed drinks can raise your blood sugar if you use juice or a regular soda as your mixer. Women should drink no more than one alcoholic drink per day, and men no more than two a day.
BELAJAR TENTANG HUBUNGAN ANTARA JENIS DAN JUMLAH KALORI MAKANAN YANG SEHAT TERHADAP PENYAKIT KENCING MANIS / GULA DARAH / DIABETES
Berikut merupakan kutipan ilmiah dari media online kesehatan yang sangat bermanfaat bagi Penulis sehingga digunakan sebagai referensi pribadi.
Diabetes-Savvy Meals in a Glance
When you're facing type 2 diabetes, eating a good balance of protein, carbohydrates, and healthy fats is important. And some people find it helpful to count carbs, too. So what's a well-balanced dinner? A power breakfast? Browse our gallery to see in a glance which meals don't quite measure up and tasty, better bets. See a doctor for a custom meal plan based on your individual needs.
Worse Bet: Farm Breakfast
The Count: 2,060 calories, 276 g carbs
No food is off limits with diabetes, but this brunch will blow your carb and calorie budget in a hurry. Experts suggest that meals for people with diabetes should contain 45-75 grams of carbohydrates, depending on individual goals. Body weight, activity, and medications all play a role. This meal packs enough carbs for four to five meals.
Better Bet: New American Breakfast
The Count: 294 calories, 40 g carbs
This quick meal delivers protein in a scrambled egg and just 40 carbs, mostly from fiber-rich oatmeal and blueberries. Fiber slows digestion to help prevent blood sugar spikes. People with diabetes need to watch all types of carbs: cereal, bread, rice, pasta, starchy veggies, sweets, fruit, milk, and yogurt. Total carbs should be spread across the day.
Worse Bet: Mexican Mayhem
The Count: 1,760 calories, 183 g carbs
Before one bite of burrito, you can inhale 98 grams of carbs and 810 calories in a restaurant serving of chips and salsa. If you're trying to slim down and eat less sodium -- as many people with diabetes are -- the steak adds 950 calories to the dietary wreckage. The total sodium is twice the 1,500 mg daily limit for people with diabetes.
Better Bet: Beef and Bean Enchilada
The Count: 443 calories, 48 g carbs
Lean beef and black beans make this Mexican dish a good option for a diabetic diet. The fiber in the beans can help lower blood cholesterol and control blood sugar. The recipe, from Holly Clegg's Trim & Terrific Diabetic Cooking, is full of veggies and light on cheese. Enjoy ten small corn chips (1 ounce) with a little guacamole.
Worse Bet: Southern Rib Plate
The Count: 2,510 calories, 83 g carbs
This classic Southern meal loads too many splurge foods onto one plate. Fatty pork ribs are dripping in sugary barbeque sauce and flanked by macaroni and cheese and corn on the cob. Corn is a high-carb vegetable, with about 32 grams of carbs in just one ear. The total calories exceed what many women, with or without diabetes, need for an entire day.
Better Bet: Pork Tenderloin Meal
The Count: 360 calories, 42 g carbs
Pork tenderloin is one of the leanest and most versatile cuts of meat. Here it's prepared in a Dijon mustard glaze, and served with steamed broccoli and mock mashed potatoes. Pureed cauliflower stands in beautifully for carb-heavy white potatoes. Round out the meal with a whole-wheat dinner roll.
Worse Bet: Shrimp Pasta Alfredo
The Count: 2,290 calories, 196 g carbs
A typical shrimp pasta alfredo in your local eatery can have huge portions and 73 grams of artery-clogging saturated fat. Diabetes boosts your risk for heart disease, so doctors advise limiting unhealthy, saturated fat to about 15 grams per day.
Better Bet: Shrimp, Feta Pasta
The Count: 369 calories, 48 g carbs
Low-fat shrimp and juicy, ripe tomatoes make this pasta dish a winner for everyone. Feta cheese has a tangy flavor with one-third less fat than hard cheese. Try pasta that is 50% to 100% whole grain to add the benefits of fiber: better blood sugar control and more satisfaction with fewer calories.
Worse Bet: Tuna Sandwich Meal
The Count: 1,050 calories, 183 g carbs
Lunch is just as important as other meals when you have diabetes, so don't grab just any sandwich or wrap. Ready-to-eat tuna-salad can be swimming in mayonnaise. Chips and a large sweetened drink push the total carbs to 183 grams -- six times the typical carb budget for a middle-aged woman with diabetes who is trying to slim down.
Better Bet: Turkey-Veggie Sandwich
The Count: 445 calories, 55 g carbs
A moist, tender turkey sandwich is widely available now -- on fresh, whole-grain bread, piled high with veggies. Make it a combo with fruit salad and a glass of low-fat milk for a terrific, diabetes-friendly meal. Six grams of fiber helps to control blood sugar. Milk, fruit, and veggies are all high in potassium to help lower blood pressure.
Worse Bet: Cajun Sausage Gumbo
The Count: 1,069 calories, 92 g carbs
Rotisserie chicken provides a reasonable start for a Cajun gumbo lunch, but the sausage, oily soup base, and giant corn muffin give this meal a junk food profile. Fat, saturated fat, and calories are sky high. The large corn muffin has 71 g of carbs. A mini-muffin would offer the same taste for only about nine carbs.
Better Bet: Trim Chicken Gumbo
The Count: 451 calories, 42 g carbs
Gumbos you make at home are more likely to fit within your meal plan. Louisiana cookbook author Holly Clegg offers one with reduced fat sausage, authentic Cajun flavors, brown rice, and lots of high fiber vegetables. Add a whole-grain salad medley with nuts, dried fruit, and chopped veggies.
Worse Bet: Fried Chicken Meal
The Count: 1,030 calories, 96 g carbs
Skip the fried chicken, mashed potato, and biscuit combo at your local chicken joint. Even if you order the white meat chicken breast, this carb and fat-heavy meal could wreak havoc with your blood sugar and your waistline. The sodium is more than double the daily limit for people with diabetes, which is 1,500 mg.
Better Bet: Roast Chicken Meal
The Count: 312 calories, 29 g carbs
Roast chicken is easy to make and easy on your health. Serve up 1/2 cup of breast meat, skin removed. Add sweet potatoes and asparagus for a super-nutritious meal. The potatoes are high in fiber and vitamin A, and so naturally sweet all they need is a sprinkle of cinnamon, a spice that may help control blood sugar.
Worse Bet: Hamburger Meal Deal
The Count: 2,700 calories, 309 g carbs
It's no surprise that a jumbo fast-food meal doesn't play well with your meal plan -- or any healthful diet. A bacon cheeseburger, large fries, and large soda contain more than a day's worth of carbs, 2,700 calories, and 44 grams of saturated fat. "Upsizing" and low prices make it hard to eat small portions in burger joints.

Better Bet: Asian Tuna Burger
The Count: 437 calories, 38 g carbs
This Asian Tuna Burger is a delicious burger alternative that's easy to make at home. Tuna provides a healthy dose of omega-3 fatty acids, to help protect against heart disease. Add a whole-grain bun, 1/2 cup of broccoli-carrot slaw, and a few orange slices. Skip the bun to shave 23 grams of carbs from your plate. Turkey and veggie burgers can also be good alternatives, if you check the calorie count.
Worse Bet: Fish Fry Platter
The Count: 910 calories, 92 g carbs
Fish is a cornerstone of a heart-healthy diet -- generally low in calories and high in healthy omega fatty acids, and a terrific choice for anyone -- unless it happens to be fried. The breading, oil, and excessive calories tend to cancel out the health benefits of the fish itself. Beware of fried sides, too, as well as coleslaw slathered in sugary mayonnaise dressing.
Better Bet: Grilled Fish and Veggies
The Count: 456 calories, 48 g carbs
A super meal for people with diabetes, or anyone else, begins with grilled or baked fish. A grilled corn salsa and a beet, pear, and walnut salad round out the meal. The total carbs don't go overboard (48 grams), and there's a good balance of other key nutrients needed in a diabetes-friendly meal: protein, fiber, and fat.
Worse Bet: Chinese Combo
The Count: 1,433 calories, 125 g carbs
Deep-fried egg rolls, fried rice, and a main dish dripping in oily sauce makes this meal an unhealthy choice. The total sodium in this type of meal is more than most people with diabetes should have over three days. Beware the MSG (monosodium glutamate) -- a seasoning that sends the sodium content soaring.
Better Bet: Stir Fry Your Way
The Count: 474 calories, 39 g carbs
Make your own beef and broccoli stir-fry meal, so you can choose a lean cut of beef and low-sodium soy sauce. Skip the greasy noodles and fried rice -- both options are full of carbs, calories, and fat. Load up on stir-fried veggies instead. Choose steamed instead of fried pot stickers to shave fat calories. For even less sodium, skip the soy sauce.
Senin, 27 Januari 2014
BELAJAR TENTANG MENGENAL KANKER PANKREAS
Berikut merupakan kutipan ilmiah kesehatan dari media online yang sangat bermanfaat bagi Penulis sehingga digunakan sebagai referensi pribadi.

Stage is a term used in cancer treatment to describe the extent of spread of the cancer. The stages of pancreatic cancer are used to guide treatment and to classify patients for clinical trials. The stages of pancreatic cancer are:
- Stage 0: No spread. Pancreatic cancer is limited to a single layer of cells in the pancreas. The pancreatic cancer is not visible on imaging tests or even to the naked eye.
- Stage I: Local growth. Pancreatic cancer is limited to the pancreas, but has grown to less than 2 centimeters across (stage IA) or greater than 2 centimeters (stage IB).
- Stage II: Local spread. Pancreatic cancer has grown outside the pancreas, or has spread to nearby lymph nodes.
- Stage III: Wider spread. The tumor has expanded into nearby major blood vessels or nerves but has not metastasized.
- Stage IV: Confirmed spread. Pancreatic cancer has spread to distant organs.
Determining pancreatic cancer's stage is often tricky. Imaging tests like CT scans and ultrasound provide some information, but knowing exactly how far pancreatic cancer has spread usually requires surgery.
Since surgery has risks, doctors first determine whether pancreatic cancer appears to be removable by surgery (resectable). Pancreatic cancer is then described as follows:
- Resectable: On imaging tests, pancreatic cancer hasn't spread (or at least not far), and a surgeon feels it might all be removable. About 10% of pancreatic cancers are considered resectable when first diagnosed.
- Locally advanced (unresectable): Pancreatic cancer has grown into major blood vessels on imaging tests, so the tumor can't safely be removed by surgery.
- Metastatic: Pancreatic cancer has clearly spread to other organs, so surgery cannot remove the cancer.
If pancreatic cancer is resectable, surgery followed by chemotherapy or radiation or both may extend survival.
Treating Resectable Pancreatic Cancer
People whose pancreatic cancer is considered resectable may undergo one of three surgeries:
Whipple procedure (pancreaticoduodenectomy): A surgeon removes the head of the pancreas, parts of the stomach and small intestine, some lymph nodes, the gallbladder, and the common bile duct. The remaining organs are reconnected in a new way to allow digestion. The Whipple procedure is a difficult and complicated surgery. Surgeons and hospitals that do the most operations have the best results.
About half the time, once a surgeon sees inside the abdomen, pancreatic cancer that was thought to be resectable turns out to have spread, and thus be unresectable. The Whipple procedure is not completed in these cases.
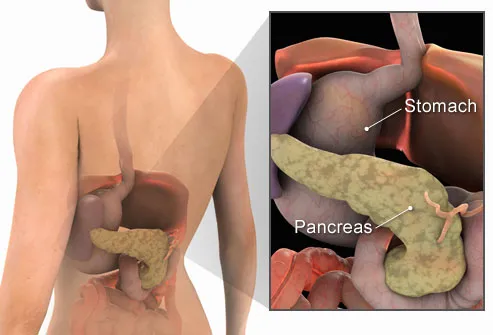
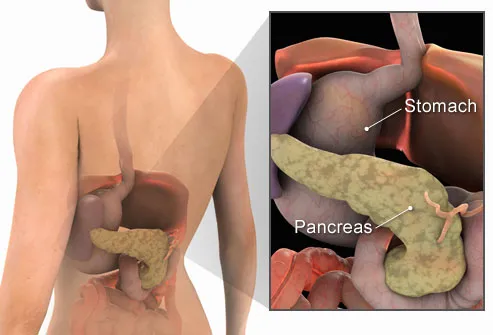
What is the Pancreas?
The pancreas is a 6-inch-long spongy, tube-shaped organ located in the back of the abdomen, behind the stomach. It has two major jobs in the body: to make digestive juices (enzymes) that help the intestines break down food, and to produce hormones -- including insulin -- that regulate the body's use of sugars and starches. Pancreatic cancer occurs when malignant (cancerous) cells grow, divide, and spread in the tissues of the pancreas.
Symptoms of Pancreatic Cancer
Pancreatic cancer is called a "silent" disease because symptoms typically do not present in the early stages. But as the cancer grows and spreads, pain often develops in the upper abdomen and sometimes spreads to the back. The pain may become worse after the person eats or lies down. Other symptoms may include jaundice, nausea, loss of appetite, weight loss, fatigue, weakness, and depression.

Causes of Pancreatic Cancer
Although the exact cause of pancreatic cancer is not known, smoking is the main risk factor, with smokers 2-3 times more likely to have the disease than nonsmokers. Age is also related, with the disease usually striking after age 45. Diabetes is also linked to pancreatic cancer, with about 10%-20% of those diagnosed with the cancer having diabetes. Other risks include chronic pancreatitis and cirrhosis of the liver. And family history of pancreatic cancer, high fat diet, obesity, and lack of exercise can also play a part.
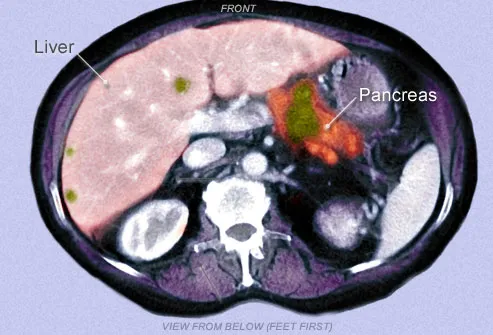
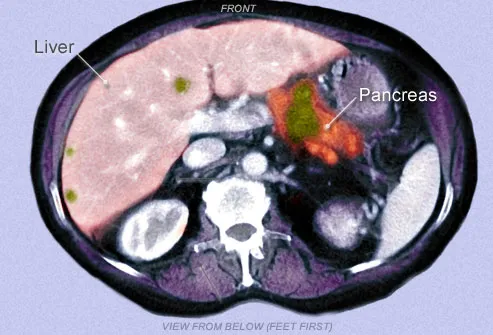
Diagnosing Pancreatic Cancer
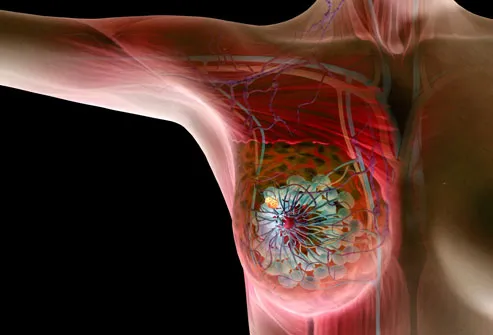
The challenge of this disease is finding it early. A doctor cannot see or feel a tumor during a routine exam. To help make the diagnosis (and determine the most appropriate treatment), imaging tests are performed (such as an ultrasound or CT scan) to view pictures of the abdomen and determine the extent of the problem. The green region shown in this colorized CT scan appears to be cancer in the pancreas and liver. The diagnosis comes from a biopsy -- taking a tissue sample from the tumor -- performed either with a needle through the skin or during an operation.
Treatment: Surgery
Surgery can cure the cancer if it has not spread past the pancreas. Since side effects depend on the extent of the surgery, the tumor is removed leaving as much of the normal pancreas intact as possible. Unfortunately, with pancreatic cancer, the malignant cells usually have spread past the pancreas at the point of diagnosis. Surgery still may be performed, even if the tumor is too large to remove. The surgery would involve procedures to help lessen some of the symptoms and prevent certain problems related to the size of the cancerous mass.
Treatment: Radiation Therapy
Radiation therapy uses high-powered radiation to kill cancer cells. Radiation is usually given five days a week for several weeks or months. This schedule helps to protect normal tissue by spreading out the total dose of radiation. Radiation is also being studied as a way to kill cancer cells that remain in the area after surgery. Radiation therapy can help relieve pain or digestive problems caused by large cancerous masses.
Treatment: Chemotherapy
Chemotherapy uses drugs to destroy cancer cells and stop them from growing or multiplying. Treatment may consist of just one drug or a combination of drugs. It may be given by mouth or by injection. The drugs enter the bloodstream and travel through the body, making chemotherapy a good choice for cancer that has spread. It is also useful after surgery to kill any cancer cells left behind.
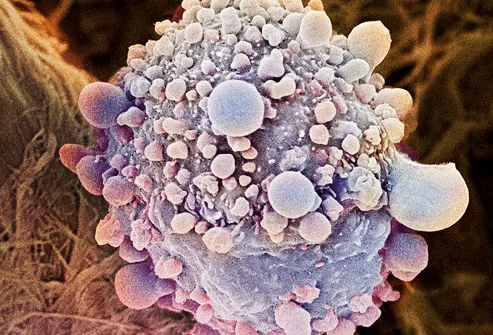
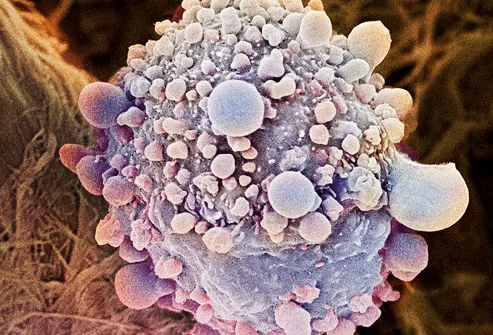
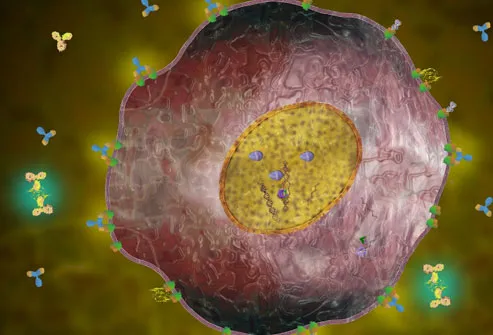
Treatment: Targeted Therapy
Newer drugs on the market have the ability to attack specific parts of the cancer cells. Targeted therapies appear to have fewer side effects than chemotherapy and are less harmful to normal cells. Targeted therapy is currently being studied for treatment of pancreatic cancer.
Shown here is a color enhanced, magnified view of a pancreatic cancer cell.
New Anticancer Treatment: Immunotherapy
Also called biological therapy, immunotherapy aims to boost a person's immune system to fight disease. Immunotherapy is not yet available for pancreatic cancer, but is being actively researched, along with the investigation into vaccines that arm the immune system to attack cancer cell.
Treatment: Palliative Therapy
Palliative therapy is used to ease symptoms and manage pain regardless of the stage of the disease or the need for other therapies. The goal of palliative care is to improve quality of life not just in the body, but in the mind and spirit. While palliative therapies are clearly appropriate at the very advanced stages of the disease, they are also helpful when given in tandem with other cancer treatments still working to fight the disease.
Getting Support
Living with pancreatic cancer isn't easy; a support system is critical to help cope with the emotional and practical aspects of this aggressive disease. Many avenues for support exist within the local community and beyond, both for the patient and their family and friends. These organizations exist to help navigate the day-to-day treatment issues and the "big picture" worries about the future.
Is Prevention Possible?
Although there's no one definite action you can take to prevent pancreatic cancer, start by avoiding the risk factors you can control.
- If you smoke, quit now.
- If your diet is high in fat, work to eat more healthfully.
- Adopt a regular exercise routine, since exercise has been shown to lower the risk of pancreatic cancer.
- Pancreatic Cancer Action Network: 877-272-6226
- American Cancer Society: 800-ACS-2345
- Cancer Care: 1-800-813-HOPE (4673)
BELAJAR TENTANG MENGENAL PENYAKIT KANKER PAYUDARA
Berikut merupakan kutipan ilmiah dari media online yang sangat bermanfaat bagi Penulis sehingga digunakan sebagai referensi pribadi.


There are often no symptoms of breast cancer, but sometimes women may discover a breast problem on their own. Signs and symptoms to be aware of may include:
- A painless lump in the breast
- Changes in breast size or shape
- Swelling in the armpit
- Nipple changes or discharge
Breast pain can also be a symptom of cancer, but this is not common.
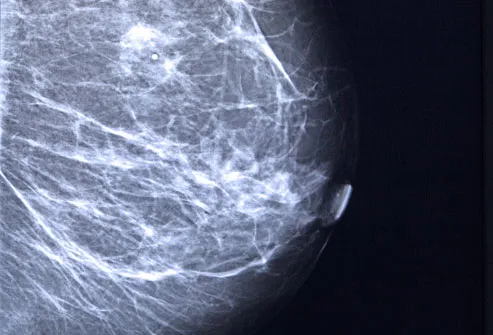
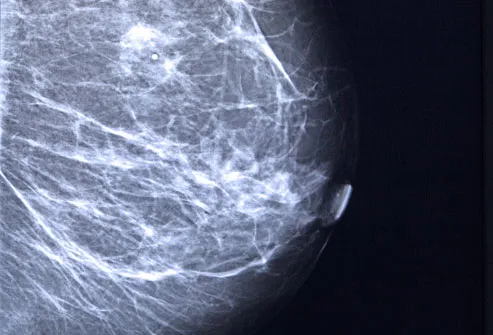
Breast Cancer and Mammograms
The earlier breast cancer is found, the easier it is to treat. And mammograms, X-rays of the breast, can detect tumors before they are large enough to feel. The American Cancer Societyrecommends yearly mammograms beginning at age 40 for women at average risk. The U.S. Preventive Services Task Force recommends a screening mammogram every two years from age 50 to 74. It also notes that before age 50, each woman should check with a doctor to find out what screening schedule is right for her, considering the potential benefits and harms.
Signs of Inflammatory Breast Cancer
Inflammatory breast cancer is a rare, fast-growing type of cancer that often causes no distinct lump. Instead, breast skin may become thick, red, and may look pitted -- like an orange peel. The area may also feel warm or tender and have small bumps that look like a rash.
Breast Ultrasound and MRI
Besides a mammogram, your doctor may order additional imaging with breast ultrasound. An ultrasound can help determine the presence of cysts, fluid-filled sacs that are not cancer. An MRI may be recommended along with a mammogram for routine screening in certain women who have a higher risk of breast cancer.
Breast Self-Exams
It was once widely recommended that women check their own breasts once a month. But studies suggest these breast self-exams play a very small role in finding cancer. The current thinking is that it’s more important to know your breasts and be aware of any changes, rather than checking them on a regular schedule. If you want to do breast self-exams, be sure to go over the technique with your doctor.
What If You Find a Lump?
First, don't panic. Eighty percent of breast lumps are not cancerous. Lumps often turn out to be harmless cysts or tissue changes related to your menstrual cycle. But you should let your doctor know right away if you find anything unusual in your breast. If it is cancer, the earlier it's found the better. And if it's not, testing can give you peace of mind.
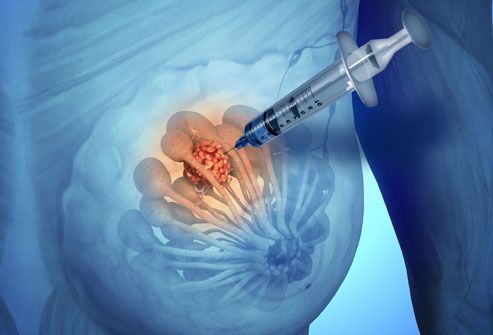
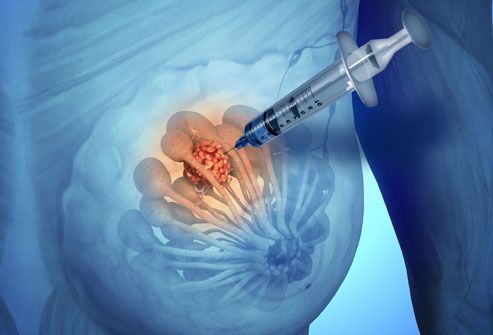
Breast Biopsy
The only sure way to determine whether a lump is cancer is to do a biopsy. This involves taking a tissue sample for further examination in the lab, sometimes through a small needle. Sometimes surgery is done to take part of or the entire lump for testing. The results will show whether the lump is cancer, and if so, what type. There are several forms of breast cancer, and treatments are carefully matched to the type of cancer.
Hormone-Sensitive Breast Cancer
Some types of breast cancer are fueled by the hormones estrogen or progesterone. A biopsy can reveal whether a tumor has receptors for estrogen (ER-positive) and/or progesterone (PR-positive). About two out of three breast cancers are hormone sensitive. There are several medications that keep the hormones from promoting further cancer growth.
The image shows a molecular model of an estrogen receptor.

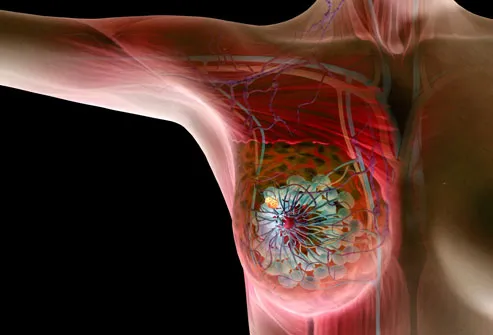
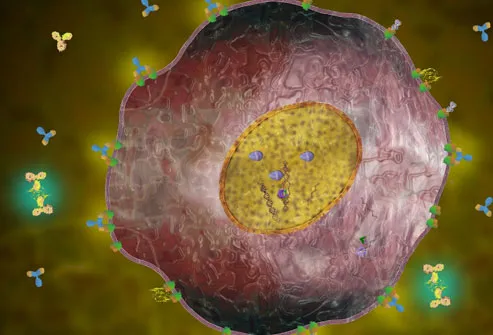
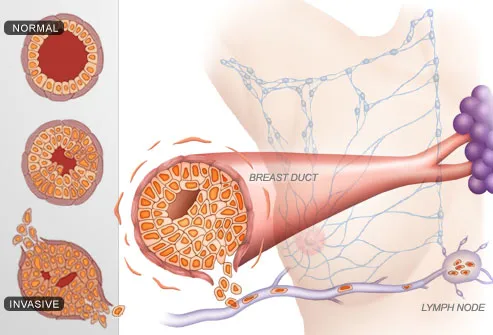
HER2-Positive Breast Cancer
In about 20% of patients, breast cancer cells have too many receptors for a protein called HER2. This type of cancer is known as HER2-positive, and it tends to spread faster than other forms of breast cancer. It's important to determine whether a tumor is HER2-positive, because there are special treatments for this form of cancer.
A HER2-positive breast cancer cell is illustrated here, with abnormal growth signals shown in green.
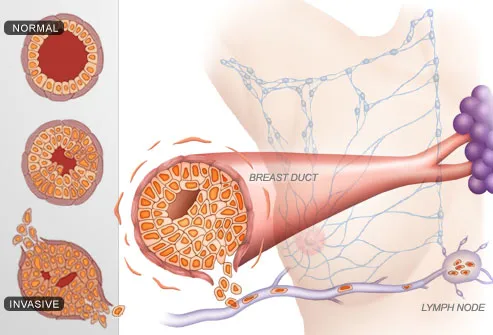
Breast Cancer Stages
Once breast cancer has been diagnosed, the next step is to determine how big the tumor is and how far the cancer has spread. This process is called staging. Doctors use Stages 0-4 to describe whether cancer is localized to the breast, has invaded nearby lymph nodes, or has spread to other organs, such as the lungs. Knowing the stage and type of breast cancer will help your health care team formulate a treatment strategy.
Breast Cancer Survival Rates
The odds of surviving breast cancer are strongly tied to how early it is found. According to the American Cancer Society, 88% of women with Stage 1 breast cancer live at least five years, compared with women who don't have cancer -- and many women in this group remain cancer-free for good. The more advanced the cancer, the lower this figure becomes. By Stage 4, the five-year relative survival rate declines to 15%. But these rates can improve as more effective treatments are found.
Breast Cancer Surgery
There are many types of breast cancer surgery, from taking out the area around the lump (lumpectomy or breast-conservation surgery) to removing the entire breast (mastectomy.) It's best to discuss the pros and cons of each of these procedures with your doctor before deciding what's right for you.

Radiation Therapy for Breast Cancer
Radiation therapy uses high-energy rays to kill cancer cells. It may be used after breast cancer surgery to wipe out any cancer cells that remain near the tumor site. It can also be used along with chemotherapy for treatment of cancer that has spread to other parts of the body. Side effects can include fatigue and swelling or a sunburn-like feeling in the treated area.
Chemotherapy for Breast Cancer
Chemotherapy uses drugs to kill cancer cells anywhere in the body. The drugs are often given by IV, but are sometimes taken by mouth or shot. Chemotherapy may be done after surgery to lower the odds of the cancer coming back. In women with advanced breast cancer, chemotherapy can help control the cancer's growth. Side effects may include hair loss, nausea, fatigue, and a higher risk of infection.
Hormone Therapy for Breast Cancer
Hormone therapy is an effective treatment for women with ER-positive or PR-positive breast cancer. These are cancers that grow more rapidly in response to the hormones estrogen or progesterone. Hormone therapy can block this effect. It is most often used after breast cancer surgery to help keep the cancer from coming back. It may also be used to reduce the chance of breast cancer developing in women who are at high risk.
Targeted Drugs for Breast Cancer
Targeted therapies are newer drugs that target specific properties within cancer cells. For example, women with HER2-positive breast cancer have too much of a protein called HER2. Targeted therapies can stop this protein from promoting the growth of cancer cells. These drugs are often used in combination with chemotherapy. They tend to have milder side effects compared with chemotherapy.
Life After Diagnosis
There's no doubt that cancer is a life-changing experience. The treatments can wear you out. You may have trouble managing daily chores, work, or social outings. This can lead to feelings of isolation. It's crucial to reach out to friends and family for support. They may be able to go with you to treatments, help out with chores, or just remind you that you are not alone. Many people choose to join a support group -- either locally or online.
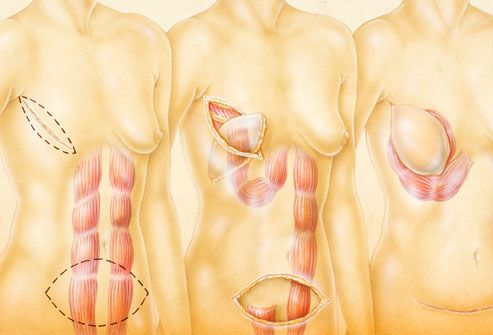
Breast Reconstruction
Many women who have a breast removed choose to undergo reconstructive surgery. This replaces the skin, nipple, and breast tissue that are lost during a mastectomy. Reconstruction can be done with a breast implant or with tissue from somewhere else in your body, such as the tummy. Some women opt to begin reconstruction at the same time as their mastectomy. But it's also possible to have reconstructive surgery months or years later.
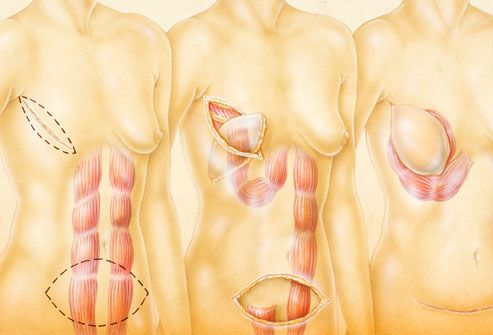
Breast Forms
An alternative to breast reconstruction is to be fitted for a breast form. This is a breast-shaped prosthesis that fits inside your bra. Wearing a breast form allows you to have a balanced look when you are dressed -- without undergoing additional surgery. Like reconstructive surgery, breast forms are often covered by insurance.
Breast Cancer: Why Me?
The most obvious risk factor for breast cancer is being a woman. Men get the disease, too, but it is about 100 times more common in women. Other top risk factors include being over age 55 or having a close relative who has had the disease. But keep in mind that up to 80% of women with breast cancer have no family history of the illness.
Breast Cancer Genes
Some women have a very high risk of breast cancer because they inherited changes in certain genes. The genes most commonly involved in breast cancer are known as BRCA1 and BRCA2. Women with mutations in these genes have up to an 80% chance of getting breast cancer at some point in life. Other genes may be linked to breast cancer risk as well.
Risk Factors in Your Control
Being overweight, getting too little exercise, and drinking more than one alcoholic beverage per day can raise the risk of developing breast cancer. Birth control pills and some forms of postmenopausal hormone therapy can also boost your risk. But the risk seems to go back to normal after these medications are stopped. Among survivors, good lifestyle choices may be helpful. Recent studies suggest that physical activity may help lower the risk of a recurrence and it's a proven mood-booster.
Langganan:
Komentar (Atom)