Iranian officials say they have confirmed the country's first two cases of MERS, a deadly virus first reported two years ago in Saudi Arabia, its neighbor on the western side of the Gulf.
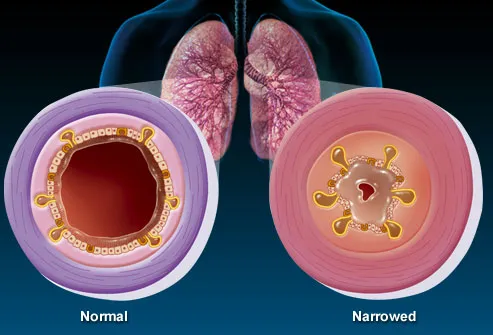
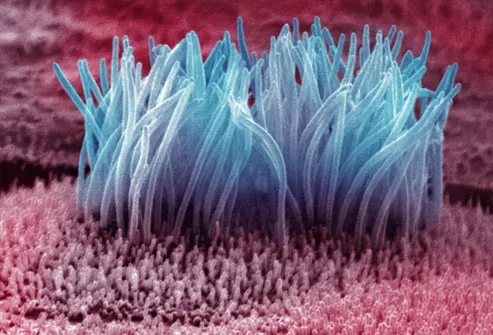
Middle East Respiratory Syndrome Corona-Virus (MERS) causes coughing, fever and sometimes fatal pneumonia, killing an estimated 30 percent of those who are infected.
An Illinois man thought to have contracted the potentially fatal MERS virus from a business associate was not infected after all, federal health officials said Wednesday.
The U.S. Centers for Disease Control and Prevention said on May 17 that the unidentified Illinois man had been infected with MERS by a man who brought the first known case of the mysterious respiratory illness to the United States in late April. That first case was a health care worker who had traveled to Saudi Arabia -- the epicenter of the MERS outbreak -- and returned to the United States before falling ill and being hospitalized in Indiana and later released.
Preliminary tests indicated that the Illinois man had tested positive for antibodies for MERS, formally called Middle East Respiratory Syndrome. Since then, however, CDC scientists tested additional blood samples and found that he was not infected with MERS. So, the Indiana MERS patient didn't spread the virus to his Illinois business associate, officials said Wednesday.
The second MERS case in the United States involved a 44-year-old health care worker from Saudi Arabia who had traveled to Orlando, Fla., where he was hospitalized and later released.
That means that the MERS virus hasn't been found in any people who had contact with the two confirmed U.S. cases, according to the CDC. There's no evidence that MERS has spread in any community setting, the CDC said.
Both of the Americans diagnosed with MERS picked up the infection in Saudi Arabia, where it is endemic.
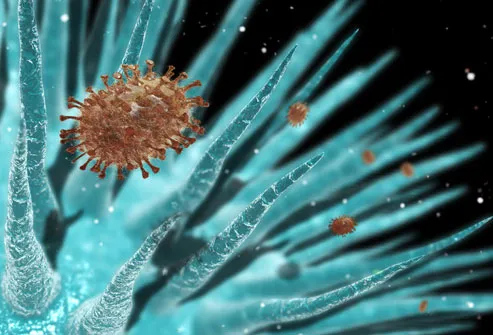
The health risk from MERS to the general public is very low, U.S. officials have said, because the virus is only passed through close contact.
The MERS virus first surfaced in 2012 in the Middle East, where most of the cases have occurred. As of May 22, 2014, there have been 632 confirmed cases and 193 deaths, according to the World Health Organization.
MERS symptoms typically include shortness of breath, coughing and fever. The illness kills about one-quarter of the people who contract the virus, according to CDC officials.
One-fifth of all MERS cases have occurred among health care workers, CDC officials have said.
In some countries, the MERS virus has spread from person to person through close contact, such as caring for or living with an infected person. But, there's currently no evidence of sustained spread of MERS in general settings, the CDC has said.
Camels have been identified as carriers of MERS, but it's not known how the virus is being spread to people.
There is no vaccine or specific treatment for MERS, which has killed more than 175 people in Saudi Arabia and spread throughout the region, also reaching as far as Malaysia, Greece, Lebanon and the United States.
"Four suspected cases of new corona virus infection were observed in a family in the province of Kerman. Two of these cases were confirmed in two sisters," said Mohammad Mahdi Gouya, the director-general of communicable diseases at the Iranian Health Ministry's Centre for Diseases Control and Prevention.
"One of the sisters is in critical condition and the other is currently receiving treatment under special circumstances," the ministry's website quoted him on Monday as saying.
A recent upsurge of infections in Saudi Arabia is of concern because of the influx of pilgrims from around the world expected in July during the Muslim fasting month of Ramadan.
Gouya also said that Tehran had dispatched trained medical teams to Saudi Arabia, where they studied MERS cases among Iranian Hajj pilgrims, according to Iran's Press TV.
Arrangements were being made for Iranian pilgrims to undergo medical check-ups after they return home, he added.
MERS is a virus from the same family as SARS, or Severe Acute Respiratory Syndrome, which killed about 800 people worldwide after it first appeared in China in 2002.