Perpustakaan Keluarga :
Helmut Todo Tua Simamora dan dr. Olga Y.V. Hutapea
Berikut merupakan kutipan ilmiah kedokteran yang sangat bermanfaat bagi Penulis sehingga disusun dan digunakan sebagai referensi pribadi.
Meningitis (from Ancient Greek μῆνιγξ/méniŋks, "membrane"[1] and the medical suffix -itis, "inflammation") is an acute inflammation of the protective membranes covering the brain and spinal cord, known collectively as the meninges.[2] The inflammation may be caused by infection with viruses, bacteria, or other microorganisms, and less commonly by certain drugs.[3] Meningitis can be life-threatening because of the inflammation's proximity to the brain and spinal cord; therefore, the condition is classified as a medical emergency.[2][4]
The most common symptoms of meningitis are headache and neck stiffness associated with fever, confusion or altered consciousness, vomiting, and an inability to tolerate light (photophobia) or loud noises (phonophobia). Children often exhibit only nonspecific symptoms, such as irritability and drowsiness. If a rash is present, it may indicate a particular cause of meningitis; for instance, meningitis caused by meningococcal bacteria may be accompanied by a characteristic rash.[2][5]
A lumbar puncture diagnoses or excludes meningitis. A needle is inserted into the spinal canal to extract a sample of cerebrospinal fluid(CSF), that envelops the brain and spinal cord. The CSF is examined in a medical laboratory.[4] The first treatment in acute meningitis consists of promptly administered antibiotics and sometimes antiviral drugs. Corticosteroids can also be used to prevent complications from excessive inflammation.[4][5] Meningitis can lead to serious long-term consequences such as deafness, epilepsy, hydrocephalusand cognitive deficits, especially if not treated quickly.[2][5] Some forms of meningitis (such as those associated with meningococci,Haemophilus influenzae type B, pneumococci or mumps virus infections) may be prevented by immunization.[2]
Signs and symptoms
Clinical features
In adults, the most common symptom of meningitis is a severe headache, occurring in almost 90% of cases of bacterial meningitis, followed by nuchal rigidity (the inability to flex the neck forward passively due to increased neck muscle tone and stiffness).[6] The classic triad of diagnostic signs consists of nuchal rigidity, sudden high fever, and altered mental status; however, all three features are present in only 44–46% of bacterial meningitis cases.[6][7] If none of the three signs are present, meningitis is extremely unlikely.[7] Other signs commonly associated with meningitis includephotophobia (intolerance to bright light) and phonophobia (intolerance to loud noises). Small children often do not exhibit the aforementioned symptoms, and may only be irritable and look unwell.[2] Thefontanelle (the soft spot on the top of a baby's head) can bulge in infants aged up to 6 months. Other features that distinguish meningitis from less severe illnesses in young children are leg pain, cold extremities, and an abnormal skin color.[8][9]
Nuchal rigidity occurs in 70% of bacterial meningitis in adults.[7] Other signs of meningism include the presence of positive Kernig's signor Brudziński sign. Kernig's sign is assessed with the person lying supine, with the hip and knee flexed to 90 degrees. In a person with a positive Kernig's sign, pain limits passive extension of the knee. A positive Brudzinski's sign occurs when flexion of the neck causes involuntary flexion of the knee and hip. Although Kernig's sign and Brudzinski's sign are both commonly used to screen for meningitis, thesensitivity of these tests is limited.[7][10] They do, however, have very good specificity for meningitis: the signs rarely occur in other diseases.[7] Another test, known as the "jolt accentuation maneuver" helps determine whether meningitis is present in those reporting fever and headache. A person is asked to rapidly rotate the head horizontally; if this does not make the headache worse, meningitis is unlikely.[7]
Meningitis caused by the bacterium Neisseria meningitidis (known as "meningococcal meningitis") can be differentiated from meningitis with other causes by a rapidly spreading petechial rash, which may precede other symptoms.[8] The rash consists of numerous small, irregular purple or red spots ("petechiae") on the trunk, lower extremities, mucous membranes, conjuctiva, and (occasionally) the palms of the hands or soles of the feet. The rash is typically non-blanching; the redness does not disappear when pressed with a finger or a glass tumbler. Although this rash is not necessarily present in meningococcal meningitis, it is relatively specific for the disease; it does, however, occasionally occur in meningitis due to other bacteria.[2] Other clues on the cause of meningitis may be the skin signs of hand, foot and mouth disease and genital herpes, both of which are associated with various forms of viral meningitis.[11]
Early complications
Additional problems may occur in the early stage of the illness. These may require specific treatment, and sometimes indicate severe illness or worse prognosis. The infection may triggersepsis, a systemic inflammatory response syndrome of falling blood pressure, fast heart rate, high or abnormally low temperature, and rapid breathing. Very low blood pressure may occur at an early stage, especially but not exclusively in meningococcal meningitis; this may lead to insufficient blood supply to other organs.[2] Disseminated intravascular coagulation, the excessive activation of blood clotting, may obstruct blood flow to organs and paradoxically increase the bleeding risk. Gangrene of limbs can occur in meningococcal disease.[2] Severe meningococcal and pneumococcal infections may result in hemorrhaging of the adrenal glands, leading to Waterhouse-Friderichsen syndrome, which is often fatal.[12]
The brain tissue may swell, pressure inside the skull may increase and the swollen brain mayherniate through the skull base. This may be noticed by a decreasing level of consciousness, loss of the pupillary light reflex, and abnormal posturing.[5] The inflammation of the brain tissue may also obstruct the normal flow of CSF around the brain (hydrocephalus).[5] Seizures may occur for various reasons; in children, seizures are common in the early stages of meningitis (in 30% of cases) and do not necessarily indicate an underlying cause.[4] Seizures may result from increased pressure and from areas of inflammation in the brain tissue.[5] Focal seizures (seizures that involve one limb or part of the body), persistent seizures, late-onset seizures and those that are difficult to control with medication indicate a poorer long-term outcome.[2]
Inflammation of the meninges may lead to abnormalities of the cranial nerves, a group of nerves arising from the brain stem that supply the head and neck area and which control, among other functions, eye movement, facial muscles, and hearing.[2][7] Visual symptoms and hearing loss may persist after an episode of meningitis.[2] Inflammation of the brain (encephalitis) or its blood vessels (cerebral vasculitis), as well as the formation of blood clots in the veins (cerebral venous thrombosis), may all lead to weakness, loss of sensation, or abnormal movement or function of the part of the body supplied by the affected area of the brain.[2][5]
Causes
Meningitis is typically caused by an infection with microorganisms. Most infections are due to viruses,[7] with bacteria, fungi, andprotozoa being the next most common causes.[3] It may also result from various non-infectious causes.[3] The term aseptic meningitisrefers to cases of meningitis in which no bacterial infection can be demonstrated. This type of meningitis is usually caused by viruses but it may be due to bacterial infection that has already been partially treated, when bacteria disappear from the meninges, or pathogens infect a space adjacent to the meninges (e.g. sinusitis). Endocarditis (an infection of the heart valves which spreads small clusters of bacteria through the bloodstream) may cause aseptic meningitis. Aseptic meningitis may also result from infection with spirochetes, a type of bacteria that includes Treponema pallidum (the cause of syphilis) and Borrelia burgdorferi (known for causing Lyme disease). Meningitis may be encountered in cerebral malaria (malaria infecting the brain) or amoebic meningitis, meningitis due to infection withamoebae such as Naegleria fowleri, contracted from freshwater sources.[3]
Bacterial
The types of bacteria that cause bacterial meningitis vary according to the infected individual's age group.
- In premature babies and newborns up to three months old, common causes are group B streptococci (subtypes III which normally inhabit the vagina and are mainly a cause during the first week of life) and bacteria that normally inhabit the digestive tract such asEscherichia coli (carrying the K1 antigen). Listeria monocytogenes (serotype IVb) may affect the newborn and occurs in epidemics.
- Older children are more commonly affected by Neisseria meningitidis (meningococcus) and Streptococcus pneumoniae (serotypes 6, 9, 14, 18 and 23) and those under five by Haemophilus influenzae type B (in countries that do not offer vaccination).[2][4]
- In adults, Neisseria meningitidis and Streptococcus pneumoniae together cause 80% of bacterial meningitis cases. Risk of infection with Listeria monocytogenes is increased in persons over 50 years old.[4][5] The introduction of pneumococcal vaccine has lowered rates of pneumococcal meningitis in both children and adults.[13]
Recent skull trauma potentially allows nasal cavity bacteria to enter the meningeal space. Similarly, devices in the brain and meninges, such as cerebral shunts, extraventricular drains or Ommaya reservoirs, carry an increased risk of meningitis. In these cases, the persons are more likely to be infected with Staphylococci, Pseudomonas, and other Gram-negative bacteria.[4] These pathogens are also associated with meningitis in people with an impaired immune system.[2] An infection in the head and neck area, such as otitis media ormastoiditis, can lead to meningitis in a small proportion of people.[4] Recipients of cochlear implants for hearing loss risk more a pneumococcal meningitis.[14]
Tuberculous meningitis, which is meningitis caused by Mycobacterium tuberculosis, is more common in people from countries wheretuberculosis is endemic, but is also encountered in persons with immune problems, such as AIDS.[15]
Recurrent bacterial meningitis may be caused by persisting anatomical defects, either congenital or acquired, or by disorders of theimmune system.[16] Anatomical defects allow continuity between the external environment and the nervous system. The most common cause of recurrent meningitis is a skull fracture,[16] particularly fractures that affect the base of the skull or extend towards the sinusesand petrous pyramids.[16] Approximately 59% of recurrent meningitis cases are due to such anatomical abnormalities, 36% are due to immune deficiencies (such as complement deficiency, which predisposes especially to recurrent meningococcal meningitis), and 5% are due to ongoing infections in areas adjacent to the meninges.[16]
Viral
Viruses that cause meningitis include enteroviruses, herpes simplex virus type 2 (and less commonly type 1), varicella zoster virus(known for causing chickenpox and shingles), mumps virus, HIV, and LCMV.[11]
Fungal
There are a number of risk factors for fungal meningitis, including the use of immunosuppressants (such as after organ transplantation),HIV/AIDS,[17] and the loss of immunity associated with aging.[18] It is uncommon in those with a normal immune system[19] but has occurred with medication contamination.[20] Symptom onset is typically more gradual, with headaches and fever being present for at least a couple of weeks before diagnosis.[18] The most common fungal meningitis is cryptococcal meningitis due to Cryptococcus neoformans.[21] In Africa, cryptococcal meningitis is estimated to be the most common cause of meningitis [22] and it accounts for 20–25% of AIDS-related deaths in Africa.[23] Other common fungal agents include Histoplasma capsulatum, Coccidioides immitis,Blastomyces dermatitidis, and Candida species.[18]
Parasitic
A parasitic cause is often assumed when there is a predominance of eosinophils (a type of white blood cell) in the CSF. The most common parasites implicated are Angiostrongylus cantonensis, Gnathostoma spinigerum, Schistosoma, as well as the conditionscysticercosis, toxocariasis, baylisascariasis, paragonimiasis, and a number of rarer infections and noninfective conditions.[24]
Non-infectious
Meningitis may occur as the result of several non-infectious causes: spread of cancer to the meninges (malignant or neoplastic meningitis)[25] and certain drugs (mainly non-steroidal anti-inflammatory drugs, antibiotics and intravenous immunoglobulins).[26] It may also be caused by several inflammatory conditions, such as sarcoidosis (which is then called neurosarcoidosis), connective tissue disorders such as systemic lupus erythematosus, and certain forms of vasculitis (inflammatory conditions of the blood vessel wall), such as Behçet's disease.[3] Epidermoid cysts and dermoid cysts may cause meningitis by releasing irritant matter into the subarachnoid space.[3][16] Mollaret's meningitis is a syndrome of recurring episodes of aseptic meningitis; it is thought to be caused by herpes simplex virus type 2. Rarely, migraine may cause meningitis, but this diagnosis is usually only made when other causes have been eliminated.[3]
Mechanism
The meninges comprise three membranes that, together with the cerebrospinal fluid, enclose and protect the brain and spinal cord (thecentral nervous system). The pia mater is a very delicate impermeable membrane that firmly adheres to the surface of the brain, following all the minor contours. The arachnoid mater (so named because of its spider-web-like appearance) is a loosely fitting sac on top of the pia mater. The subarachnoid space separates the arachnoid and pia mater membranes and is filled with cerebrospinal fluid. The outermost membrane, the dura mater, is a thick durable membrane, which is attached to both the arachnoid membrane and the skull.
In bacterial meningitis, bacteria reach the meninges by one of two main routes: through the bloodstream or through direct contact between the meninges and either the nasal cavity or the skin. In most cases, meningitis follows invasion of the bloodstream by organisms that live upon mucous surfaces such as the nasal cavity. This is often in turn preceded by viral infections, which break down the normal barrier provided by the mucous surfaces. Once bacteria have entered the bloodstream, they enter the subarachnoid space in places where the blood–brain barrier is vulnerable—such as the choroid plexus. Meningitis occurs in 25% of newborns with bloodstream infections due to group B streptococci; this phenomenon is less common in adults.[2] Direct contamination of the cerebrospinal fluid may arise from indwelling devices, skull fractures, or infections of the nasopharynx or the nasal sinuses that have formed a tract with the subarachnoid space (see above); occasionally, congenital defects of the dura mater can be identified.[2]
The large-scale inflammation that occurs in the subarachnoid space during meningitis is not a direct result of bacterial infection but can rather largely be attributed to the response of the immune system to the entry of bacteria into the central nervous system. When components of the bacterial cell membrane are identified by the immune cells of the brain (astrocytes and microglia), they respond by releasing large amounts of cytokines, hormone-like mediators that recruit other immune cells and stimulate other tissues to participate in an immune response. The blood–brain barrier becomes more permeable, leading to "vasogenic" cerebral edema (swelling of the brain due to fluid leakage from blood vessels). Large numbers of white blood cells enter the CSF, causing inflammation of the meninges and leading to "interstitial" edema (swelling due to fluid between the cells). In addition, the walls of the blood vessels themselves become inflamed (cerebral vasculitis), which leads to decreased blood flow and a third type of edema, "cytotoxic" edema. The three forms of cerebral edema all lead to increased intracranial pressure; together with the lowered blood pressure often encountered in acute infection, this means that it is harder for blood to enter the brain, consequently brain cells are deprived of oxygen and undergo apoptosis (automatedcell death).[2]
It is recognized that administration of antibiotics may initially worsen the process outlined above, by increasing the amount of bacterial cell membrane products released through the destruction of bacteria. Particular treatments, such as the use of corticosteroids, are aimed at dampening the immune system's response to this phenomenon.[2][5]
Diagnosis
| Type of meningitis | Glucose | Protein | Cells |
|---|---|---|---|
| Acute bacterial | low | high | PMNs, often > 300/mm³ |
| Acute viral | normal | normal or high | mononuclear, < 300/mm³ |
| Tuberculous | low | high | mononuclear and PMNs, < 300/mm³ |
| Fungal | low | high | < 300/mm³ |
| Malignant | low | high | usually mononuclear |
Blood tests and imaging
In someone suspected of having meningitis, blood tests are performed for markers of inflammation (e.g. C-reactive protein, complete blood count), as well as blood cultures.[4][28]
The most important test in identifying or ruling out meningitis is analysis of the cerebrospinal fluid through lumbar puncture (LP, spinal tap).[29]However, lumbar puncture is contraindicated if there is a mass in the brain (tumor or abscess) or the intracranial pressure (ICP) is elevated, as it may lead to brain herniation. If someone is at risk for either a mass or raised ICP (recent head injury, a known immune system problem, localizing neurological signs, or evidence on examination of a raised ICP), a CT or MRI scan is recommended prior to the lumbar puncture.[4][28][30] This applies in 45% of all adult cases.[5] If a CT or MRI is required before LP, or if LP proves difficult, professional guidelines suggest that antibiotics should be administered first to prevent delay in treatment,[4] especially if this may be longer than 30 minutes.[28][30] Often, CT or MRI scans are performed at a later stage to assess for complications of meningitis.[2]
In severe forms of meningitis, monitoring of blood electrolytes may be important; for example, hyponatremia is common in bacterial meningitis, due to a combination of factors, including dehydration, the inappropriate excretion of the antidiuretic hormone (SIADH), or overly aggressive intravenous fluid administration.[5][31]
The most important test in identifying or ruling out meningitis is analysis of the cerebrospinal fluid through lumbar puncture (LP, spinal tap).[29]However, lumbar puncture is contraindicated if there is a mass in the brain (tumor or abscess) or the intracranial pressure (ICP) is elevated, as it may lead to brain herniation. If someone is at risk for either a mass or raised ICP (recent head injury, a known immune system problem, localizing neurological signs, or evidence on examination of a raised ICP), a CT or MRI scan is recommended prior to the lumbar puncture.[4][28][30] This applies in 45% of all adult cases.[5] If a CT or MRI is required before LP, or if LP proves difficult, professional guidelines suggest that antibiotics should be administered first to prevent delay in treatment,[4] especially if this may be longer than 30 minutes.[28][30] Often, CT or MRI scans are performed at a later stage to assess for complications of meningitis.[2]
In severe forms of meningitis, monitoring of blood electrolytes may be important; for example, hyponatremia is common in bacterial meningitis, due to a combination of factors, including dehydration, the inappropriate excretion of the antidiuretic hormone (SIADH), or overly aggressive intravenous fluid administration.[5][31]
Lumbar puncture
A lumbar puncture is done by positioning the person, usually lying on the side, applying local anesthetic, and inserting a needle into the dural sac (a sac around the spinal cord) to collect cerebrospinal fluid (CSF). When this has been achieved, the "opening pressure" of the CSF is measured using a manometer. The pressure is normally between 6 and 18 cm water (cmH2O);[29] in bacterial meningitis the pressure is usually elevated.[4][28] In cryptococcal meningitis, intracranial pressure is markedly elevated.[32] The initial appearance of the fluid may prove an indication of the nature of the infection: cloudy CSF indicates higher levels of protein, white and red blood cells and/or bacteria, and therefore may suggest bacterial meningitis.[4]
The CSF sample is examined for presence and types of white blood cells, red blood cells, proteincontent and glucose level.[4] Gram staining of the sample may demonstrate bacteria in bacterial meningitis, but absence of bacteria does not exclude bacterial meningitis as they are only seen in 60% of cases; this figure is reduced by a further 20% if antibiotics were administered before the sample was taken. Gram staining is also less reliable in particular infections such as listeriosis.Microbiological culture of the sample is more sensitive (it identifies the organism in 70–85% of cases) but results can take up to 48 hours to become available.[4] The type of white blood cell predominantly present (see table) indicates whether meningitis is bacterial (usually neutrophil-predominant) or viral (usually lymphocyte-predominant),[4] although at the beginning of the disease this is not always a reliable indicator. Less commonly, eosinophils predominate, suggesting parasitic or fungal etiology, among others.[24]
The concentration of glucose in CSF is normally above 40% of that in blood. In bacterial meningitis it is typically lower; the CSF glucose level is therefore divided by the blood glucose (CSF glucose to serum glucose ratio). A ratio ≤0.4 is indicative of bacterial meningitis;[29]in the newborn, glucose levels in CSF are normally higher, and a ratio below 0.6 (60%) is therefore considered abnormal.[4] High levels oflactate in CSF indicate a higher likelihood of bacterial meningitis, as does a higher white blood cell count.[29] If lactate levels are less than 35 mg/dl and the person has not previously received antibiotics then this may rule out bacterial meningitis.[33]
Various other specialized tests may be used to distinguish between different types of meningitis. A latex agglutination test may be positive in meningitis caused by Streptococcus pneumoniae, Neisseria meningitidis, Haemophilus influenzae, Escherichia coli and group B streptococci; its routine use is not encouraged as it rarely leads to changes in treatment, but it may be used if other tests are not diagnostic. Similarly, the limulus lysate test may be positive in meningitis caused by Gram-negative bacteria, but it is of limited use unless other tests have been unhelpful.[4] Polymerase chain reaction (PCR) is a technique used to amplify small traces of bacterial DNA in order to detect the presence of bacterial or viral DNA in cerebrospinal fluid; it is a highly sensitive and specific test since only trace amounts of the infecting agent's DNA is required. It may identify bacteria in bacterial meningitis and may assist in distinguishing the various causes of viral meningitis (enterovirus, herpes simplex virus 2 and mumps in those not vaccinated for this).[11] Serology(identification of antibodies to viruses) may be useful in viral meningitis.[11] If tuberculous meningitis is suspected, the sample is processed for Ziehl-Neelsen stain, which has a low sensitivity, and tuberculosis culture, which takes a long time to process; PCR is being used increasingly.[15] Diagnosis of cryptococcal meningitis can be made at low cost using an India ink stain of the CSF; however, testing for cryptococcal antigen in blood or CSF is more sensitive, particularly in people with AIDS.[34][35]
A diagnostic and therapeutic difficulty is "partially treated meningitis", where there are meningitis symptoms after receiving antibiotics (such as for presumptive sinusitis). When this happens, CSF findings may resemble those of viral meningitis, but antibiotic treatment may need to be continued until there is definitive positive evidence of a viral cause (e.g. a positive enterovirus PCR).[11]
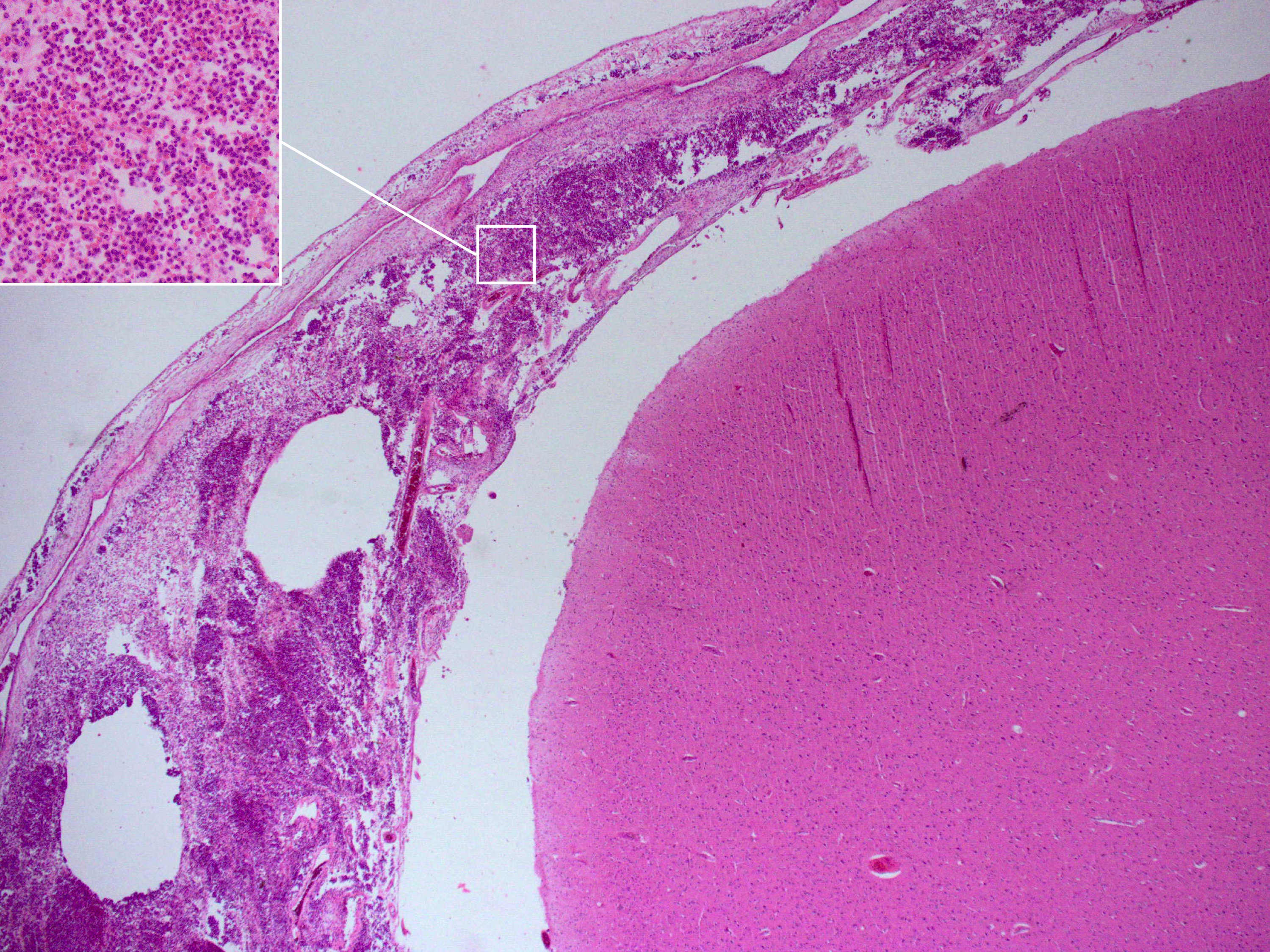
Postmortem
Meningitis can be diagnosed after death has occurred. The findings from a post mortem are usually a widespread inflammation of the pia mater and arachnoid layers of the meninges. Neutrophil granulocytes tend to have migrated to the cerebrospinal fluid and the base of the brain, along withcranial nerves and the spinal cord, may be surrounded with pus — as may the meningeal vessels.[36]
Prevention
For some causes of meningitis, protection can be provided in the long term through vaccination, or in the short term with antibiotics. Some behavioral measures may also be effective.
Behavioral
Bacterial and viral meningitis are contagious; however, neither is as contagious as the common coldor flu.[37] Both can be transmitted through droplets of respiratory secretions during close contact such as kissing, sneezing or coughing on someone, but cannot be spread by only breathing the air where a person with meningitis has been.[37] Viral meningitis is typically caused by enteroviruses, and is most commonly spread through fecal contamination.[37] The risk of infection can be decreased by changing the behavior that led to transmission.
Vaccination
Since the 1980s, many countries have included immunization against Haemophilus influenzae type B in their routine childhood vaccination schemes. This has practically eliminated this pathogen as a cause of meningitis in young children in those countries. In the countries where the disease burden is highest, however, the vaccine is still too expensive.[38][39] Similarly, immunization against mumps has led to a sharp fall in the number of cases of mumps meningitis, which prior to vaccination occurred in 15% of all cases of mumps.[11]
Meningococcus vaccines exist against groups A, C, W135 and Y.[40] In countries where the vaccine for meningococcus group C was introduced, cases caused by this pathogen have decreased substantially.[38] A quadrivalent vaccine now exists, which combines all four vaccines. Immunization with the ACW135Y vaccine against four strains is now a visa requirement for taking part in Hajj.[41] Development of a vaccine against group B meningococci has proved much more difficult, as its surface proteins (which would normally be used to make a vaccine) only elicit a weak response from the immune system, or cross-react with normal human proteins.[38][40] Still, some countries (New Zealand, Cuba, Norway and Chile) have developed vaccines against local strains of group B meningococci; some have shown good results and are used in local immunization schedules.[40] In Africa, until recently, the approach for prevention and control of meningococcal epidemics was based on early detection of the disease and emergency reactive mass vaccination of the at-risk population with bivalent A/C or trivalent A/C/W135 polysaccharide vaccines,[42] though the introduction of MenAfriVac (meningococcus group A vaccine) has demonstrated effectiveness in young people and has been described as a model for product development partnerships in resource-limited settings.[43][44]
Routine vaccination against Streptococcus pneumoniae with the pneumococcal conjugate vaccine (PCV), which is active against seven common serotypes of this pathogen, significantly reduces the incidence of pneumococcal meningitis.[38][45] The pneumococcal polysaccharide vaccine, which covers 23 strains, is only administered to certain groups (e.g. those who have had a splenectomy, the surgical removal of the spleen); it does not elicit a significant immune response in all recipients, e.g. small children.[45] Childhood vaccination with Bacillus Calmette-Guérin has been reported to significantly reduce the rate of tuberculous meningitis, but its waning effectiveness in adulthood has prompted a search for a better vaccine.[38]
Antibiotics
Short-term antibiotic prophylaxis is another method of prevention, particularly of meningococcal meningitis. In cases of meningococcal meningitis, prophylactic treatment of close contacts with antibiotics (e.g. rifampicin, ciprofloxacin or ceftriaxone) can reduce their risk of contracting the condition, but does not protect against future infections.[28][46] Resistance to rifampicin has been noted to increase after use, which has caused some to recommend considering other agents.[46] While antibiotics are frequently used in an attempt to prevent meningitis in those with a basilar skull fracture there is insufficient evidence to determine whether this is beneficial or harmful.[47] This applies to those with or without a CSF leak.[47]
Management
Meningitis is potentially life-threatening and has a high mortality rate if untreated;[4] delay in treatment has been associated with a poorer outcome.[5] Thus, treatment with wide-spectrum antibiotics should not be delayed while confirmatory tests are being conducted.[30] If meningococcal disease is suspected in primary care, guidelines recommend that benzylpenicillin be administered before transfer to hospital.[8] Intravenous fluids should be administered if hypotension (low blood pressure) or shock are present.[30] Given that meningitis can cause a number of early severe complications, regular medical review is recommended to identify these complications early[30] and to admit the person to an intensive care unit if deemed necessary.[5]
Mechanical ventilation may be needed if the level of consciousness is very low, or if there is evidence of respiratory failure. If there are signs of raised intracranial pressure, measures to monitor the pressure may be taken; this would allow the optimization of the cerebral perfusion pressure and various treatments to decrease the intracranial pressure with medication (e.g. mannitol).[5] Seizures are treated with anticonvulsants.[5] Hydrocephalus (obstructed flow of CSF) may require insertion of a temporary or long-term drainage device, such as a cerebral shunt.[5]
Bacterial meningitis
Antibiotics
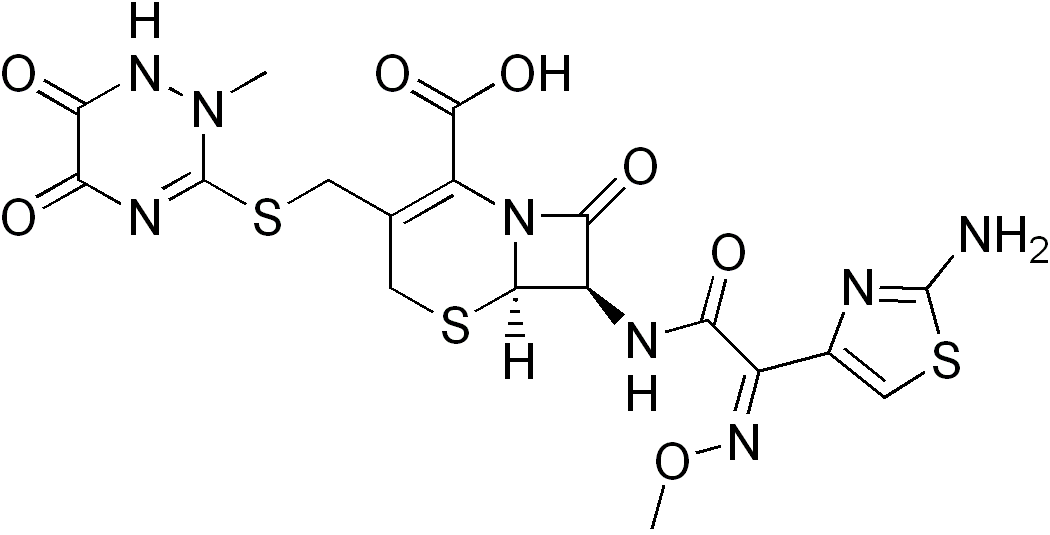
Empiric antibiotics (treatment without exact diagnosis) should be started immediately, even before the results of the lumbar puncture and CSF analysis are known. The choice of initial treatment depends largely on the kind of bacteria that cause meningitis in a particular place and population. For instance, in the United Kingdom empirical treatment consists of a third-generation cefalosporin such as cefotaxime or ceftriaxone.[28][30] In the USA, where resistance to cefalosporins is increasingly found in streptococci, addition of vancomycin to the initial treatment is recommended.[4][5][28]Chloramphenicol, either alone or in combination with ampicillin, however, appears to work equally well.[48]
Empirical therapy may be chosen on the basis of the person's age, whether the infection was preceded by a head injury, whether the person has undergone recent neurosurgery and whether or not a cerebral shunt is present.[4] In young children and those over 50 years of age, as well as those who are immunocompromised, the addition of ampicillin is recommended to cover Listeria monocytogenes.[4][28] Once the Gram stain results become available, and the broad type of bacterial cause is known, it may be possible to change the antibiotics to those likely to deal with the presumed group of pathogens.[4] The results of the CSF culture generally take longer to become available (24–48 hours). Once they do, empiric therapy may be switched to specific antibiotic therapy targeted to the specific causative organism and its sensitivities to antibiotics.[4] For an antibiotic to be effective in meningitis it must not only be active against the pathogenic bacterium but also reach the meninges in adequate quantities; some antibiotics have inadequate penetrance and therefore have little use in meningitis. Most of the antibiotics used in meningitis have not been tested directly on people with meningitis in clinical trials. Rather, the relevant knowledge has mostly derived from laboratory studies in rabbits.[4] Tuberculous meningitis requires prolonged treatment with antibiotics. While tuberculosis of the lungs is typically treated for six months, those with tuberculous meningitis are typically treated for a year or longer.[15]
Steroids
Adjuvant treatment with corticosteroids (usually dexamethasone) has shown some benefits, such as a reduction of hearing loss,[49] and better short term neurological outcomes[50] in adolescents and adults from high-income countries with low rates of HIV.[51] Some research has found reduced rates of death[51] while other research has not.[50] They also appear to be beneficial in those with tuberculosis meningitis, at least in those who are HIV negative.[52]
Professional guidelines therefore recommend the commencement of dexamethasone or a similar corticosteroid just before the first dose of antibiotics is given, and continued for four days.[28][30] Given that most of the benefit of the treatment is confined to those with pneumococcal meningitis, some guidelines suggest that dexamethasone be discontinued if another cause for meningitis is identified.[4][28] The likely mechanism is suppression of overactive inflammation.[53]
Adjuvant corticosteroids have a different role in children than in adults. Though the benefit of corticosteroids has been demonstrated in adults as well as in children from high-income countries, their use in children from low-income countries is not supported by the evidence; the reason for this discrepancy is not clear.[50] Even in high-income countries, the benefit of corticosteroids is only seen when they are given prior to the first dose of antibiotics, and is greatest in cases of H. influenzae meningitis,[4][54] the incidence of which has decreased dramatically since the introduction of the Hib vaccine. Thus, corticosteroids are recommended in the treatment of pediatric meningitis if the cause is H. influenzae, and only if given prior to the first dose of antibiotics; other uses are controversial.[4]
Viral meningitis
Viral meningitis typically only requires supportive therapy; most viruses responsible for causing meningitis are not amenable to specific treatment. Viral meningitis tends to run a more benign course than bacterial meningitis. Herpes simplex virus and varicella zoster virusmay respond to treatment with antiviral drugs such as aciclovir, but there are no clinical trials that have specifically addressed whether this treatment is effective.[11] Mild cases of viral meningitis can be treated at home with conservative measures such as fluid, bedrest, and analgesics.[55]
Fungal meningitis
Fungal meningitis, such as cryptococcal meningitis, is treated with long courses of high dose antifungals, such as amphotericin B andflucytosine.[34][56] Raised intracranial pressure is common in fungal meningitis, and frequent (ideally daily) lumbar punctures to relieve the pressure are recommended,[34] or alternatively a lumbar drain.[32]
Prognosis
Untreated, bacterial meningitis is almost always fatal. Viral meningitis, in contrast, tends to resolve spontaneously and is rarely fatal. With treatment, mortality (risk of death) from bacterial meningitis depends on the age of the person and the underlying cause. Of newborns, 20–30% may die from an episode of bacterial meningitis. This risk is much lower in older children, whose mortality is about 2%, but rises again to about 19–37% in adults.[2][5] Risk of death is predicted by various factors apart from age, such as the pathogen and the time it takes for the pathogen to be cleared from the cerebrospinal fluid,[2] the severity of the generalized illness, a decreased level of consciousness or an abnormally low count of white blood cells in the CSF.[5] Meningitis caused by H. influenzae and meningococci has a better prognosis than cases caused by group B streptococci, coliforms and S. pneumonia.[2] In adults, too, meningococcal meningitis has a lower mortality (3–7%) than pneumococcal disease.[5]
In children there are several potential disabilities which may result from damage to the nervous system, including sensorineural hearing loss, epilepsy, learning and behavioral difficulties, as well as decreased intelligence.[2] These occur in about 15% of survivors.[2] Some of the hearing loss may be reversible.[58] In adults, 66% of all cases emerge without disability. The main problems are deafness(in 14%) and cognitive impairment (in 10%).[5]
Epidemiology
Although meningitis is a notifiable disease in many countries, the exact incidence rate is unknown.[11] As of 2010 it is estimated that it resulted in 420,000 deaths.[59]
Bacterial meningitis occurs in about 3 people per 100,000 annually in Western countries. Population-wide studies have shown that viral meningitis is more common, at 10.9 per 100,000, and occurs more often in the summer. In Brazil, the rate of bacterial meningitis is higher, at 45.8 per 100,000 annually.[7] Sub-Saharan Africa has been plagued by large epidemics of meningococcal meningitis for over a century,[60] leading to it being labeled the "meningitis belt". Epidemics typically occur in the dry season (December to June), and an epidemic wave can last two to three years, dying out during the intervening rainy seasons.[61] Attack rates of 100–800 cases per 100,000 are encountered in this area,[62] which is poorly served by medical care. These cases are predominantly caused by meningococci.[7] The largest epidemic ever recorded in history swept across the entire region in 1996–1997, causing over 250,000 cases and 25,000 deaths.[63]
Meningococcal disease occurs in epidemics in areas where many people live together for the first time, such as army barracks during mobilization, college campuses[2] and the annual Hajj pilgrimage.[41] Although the pattern of epidemic cycles in Africa is not well understood, several factors have been associated with the development of epidemics in the meningitis belt. They include: medical conditions (immunological susceptibility of the population), demographic conditions (travel and large population displacements), socioeconomic conditions (overcrowding and poor living conditions), climatic conditions (drought and dust storms), and concurrent infections (acute respiratory infections).[62]
There are significant differences in the local distribution of causes for bacterial meningitis. For instance, while N. meningitides groups B and C cause most disease episodes in Europe, group A is found in Asia and continues to predominate in Africa, where it causes most of the major epidemics in the meningitis belt, accounting for about 80% to 85% of documented meningococcal meningitis cases.[62]
History
Some suggest that Hippocrates may have realized the existence of meningitis,[7] and it seems that meningism was known to pre-Renaissance physicians such as Avicenna.[64] The description of tuberculous meningitis, then called "dropsy in the brain", is often attributed to Edinburgh physician Sir Robert Whytt in a posthumous report that appeared in 1768, although the link with tuberculosis and its pathogen was not made until the next century.[64][65]
It appears that epidemic meningitis is a relatively recent phenomenon.[66] The first recorded major outbreak occurred in Geneva in 1805.[66][67] Several other epidemics in Europe and the United States were described shortly afterward, and the first report of an epidemic in Africa appeared in 1840. African epidemics became much more common in the 20th century, starting with a major epidemic sweeping Nigeria and Ghana in 1905–1908.[66]
The first report of bacterial infection underlying meningitis was by the Austrian bacteriologist Anton Weichselbaum, who in 1887 described the meningococcus.[68] Mortality from meningitis was very high (over 90%) in early reports. In 1906, antiserum was produced in horses; this was developed further by the American scientist Simon Flexner and markedly decreased mortality from meningococcal disease.[69][70] In 1944, penicillin was first reported to be effective in meningitis.[71] The introduction in the late 20th century ofHaemophilus vaccines led to a marked fall in cases of meningitis associated with this pathogen,[39] and in 2002, evidence emerged that treatment with steroids could improve the prognosis of bacterial meningitis.[50][53][70]
An outbreak of meningococcal disease has sickened four students at a major California university, prompting discussions with federal regulators about using a vaccine approved for use in Europe but not in the United States.
They were stricken by a form of the bacteria that does not respond to the meningitis vaccine currently approved for use in the United States, said the spokeswoman, Susan Klein-Rothschild.
A vaccine known to be effective against this form of meningitis is approved for use in Europe, and Santa Barbara public health officials were in discussions with the federal Centers for Disease Control and Prevention about using it to protect students at the California university.
The discussions come after federal officials agreed to allow Princeton University in New Jersey to administer the European vaccine, Bexsero, after eight students there were diagnosed with similar infections since March.
The CDC is monitoring the California cases and evaluating whether to request similar permission from the Food and Drug Administration to vaccinate the Santa Barbara students with Bexsero, said Dr. Tom Clark, head of meningitis surveillance at the federal health agency.
Blood samples from the infected students are being tested at the CDC's Atlanta headquarters to see if the bacteria responds to the European vaccine, Clark said. Officials were also watching to see if the Santa Barbara outbreak continues to grow.
"It's an exceptional thing, really, to use an unlicensed vaccine in an outbreak like this," Clark said. "We want to be certain that the antibodies that you get from the vaccine actually kill these bacteria."
GAP IN PROTECTIONThe type of the disease infecting the Princeton and Santa Barbara students accounts for about a third of meningococcal disease cases in the United States, and a vaccine that targets more strains of the bacteria is not likely to be approved for several years, Clark said.
"It really has been a gap in our ability to protect against meningococcal disease," Clark said. "Everybody has really been looking forward to the day that there would be a licensed vaccine."
Overall, outbreaks of meningitis have declined significantly in the United States since vaccinations for four strains of the bacteria were recommended for all teenagers in 2005, he said.
Meningitis, which causes the brain and spinal cord to swell, is spread through coughing and exchanges of saliva, and people living in dormitories or other crowded living quarters are especially at risk.
Infections once plagued five to 10 of every 100,000 college-aged adults, but now just one per million becomes ill. Incidence of serogroup B, the type infecting the Santa Barbara and Princeton students, has dropped along with the others, Clark said.
The most severe cases can result in death, hearing loss, brain damage, kidney disease or amputation of limbs.
In the Santa Barbara cases, one student has been left permanently disabled, Klein-Rothschild said, declining to provide further details on the case, citing privacy issues.
To prevent additional cases, Santa Barbara public health officials will provide the antibiotic Cipro to students and others who may have been exposed to the bacteria.
The university is also suspending social events by fraternities and sororities, saying the parties put too many students in close quarters and could cause the outbreak to spread further.
Students and faculty can also protect themselves by maintaining good hygiene and nutrition, and getting plenty of sleep during the stressful exam period, which begins this month, Klein-Rothschild said.
Bexsero, made by Swiss drugmaker Novartis, is designed to protect against serogroup B, a strain of meningococcal infection that is not as common in the United States as it is in other parts of the world.
Drexel University confirmed on Friday that a student died this week from the rare strain of meningitis that hit Princeton University and the University of California at Santa Barbara last fall.
Stephanie Ross, 19, a mechanical engineering major from the Pittsburgh area, was found unresponsive in her room at Phi Mu sorority last week, according to a letter sent to the university community by school President John Fry. Lab tests confirmed that the rare "serogroup B" strain was responsible for her death, the university said in a statement.
Drexel, located in downtown Philadelphia, is tracking down anyone who had recent contact with Ross in an effort to provide prophylactic antibiotics to ward off infection, school officials said in a statement.
Ross recently attended a regional officer training conference for the Phi Mu sorority. The sorority's national chapter said in a statement that it has contacted other conference attendees.
Meningitis is generally spread through close personal contact such as kissing, sharing drinks or coughing. Most college students are required to get a meningitis vaccination, but that does not protect against this particular strain.
After eight students were infected at Princeton University, the U.S. Food and Drug Administration in November allowed the school to import a vaccine that is not approved in the United States but is licensed in Europe and Australia.
In February, students at the University of California at Santa Barbara began receiving the vaccine - known as Bexsero - after an outbreak sickened four and led to one student having a foot amputated.
No one died at either school.
The U.S. Centers for Disease Control and Prevention says there are about 160 serotype B infections in the United States every year.
Sunil Shah, 19, a biomedical engineering student at Drexel, said students on Friday were made aware of the death and the risk to those who were in contact with Ross, but were going about their daily business.
"I know the school is taking it seriously because they've sent several emails," he said.
Experts have recommended that the UK government introduces a vaccine against meningitis B for babies, in a move welcomed by scientists and charities.
1. What has happened?
The Joint Committee on Vaccination and Immunisation (JCVI), the expert body that advises the government on vaccinations, has recommended babies be given the meningitis B vaccine, from two months of age.
Last year the committee ruled in an interim report that the vaccine should not be introduced - because, it said, it was not cost effective.
This caused an outcry from campaigners, and in January 118 paediatricians, nurses and scientists wrote to Jeremy Hunt, the health secretary, pressing for the committee to reconsider.
The backing for the Bexsero vaccine, manufactured by Novartis, is on condition that it can be delivered on a "cost-effective" basis.
2. What is meningitis B?

It is a bacterial infection that usually affects children under one year old.
There are about 1,870 cases each year in the UK.
Symptoms include a high fever with cold hands and feet, confusion, vomiting and headaches,
With early diagnosis and antibiotic treatment, most will make a full recovery.
But it is fatal in one in 10 cases - and about one in four of those who survive are left with long-term problems, such as amputation, deafness, epilepsy and learning difficulties.
Meningitis is an infection of the meninges - the membrane that surrounds the brain and spinal cord.
There are effective vaccines against other strains of meningitis - but until now not against Meningitis B.
3. Is the vaccine used already?

Yes - but this decision is set to mean the UK will be the first country in the world to add the jab to its routine childhood vaccination programme.
Bexsero is already available privately in the UK.
The vaccine has been found to be safe and well tolerated in trials involving more than 8,000 people.
It is thought to provide about 73% protection against meningitis B.
4. So when will children get it?

Not just yet. The government and manufacturers Novartis will now enter into negotiations about the cost of the vaccine to the NHS in a formal procurement process.
There is no commitment to when the vaccine might be introduced.
But the government says it should be "as soon as possible", but that it "owes it to children" to ensure there is a reliable supply of vaccine which the NHS can deliver it effectively.
Pregnant women, babies and kids should not drink raw or unpasteurized milk, a group of pediatricians said on Monday.
Because of infection risks, the American Academy of Pediatrics (AAP) Committee on Infectious Diseases and Committee on Nutrition also said sales of unpasteurized milk, cheese and related products should be banned in the U.S.
Pasteurizing kills bacteria that can be present in raw milk. It involves heating the milk to at least 161 degrees Fahrenheit for more than 15 seconds and then rapidly cooling it.
"It's kind of like riding in a car with seatbelts," Kathryn Boor said. "If you've got the opportunity for a safety barrier, which would be pasteurization, why wouldn't you use it?"
Boor studies food safety at Cornell University in Ithaca, New York, where she is also the dean of Agriculture and Life Sciences. She was not involved in the new report.At least 97 percent of dairy products consumed in the U.S. are pasteurized, the committees wrote in Pediatrics, the journal of the AAP.
The U.S. Food and Drug Administration prohibits shipping raw milk for human consumption across state lines, but its sale is still legal in many states. Raw milk can carry bacteria such as E. coli and Salmonella from sick animals or contact with manure, for instance.
Still, some groups promote raw milk based on studies suggesting it is tied to a lower risk of allergies and asthma.
Boor said those studies looked at children who also spend a lot of time outside and working on farms - kids who are probably different in many ways from those who drink pasteurized milk and live in the suburbs.
"While those studies are really tempting to link (raw milk and fewer allergies), I think that the picture is considerably more complicated than that," she told Reuters Health.
Claims that raw milk has nutrients that are killed by pasteurization also haven't been supported, researchers said.
When it comes to raw milk, Boor said, "We can quantify the risks. We cannot quantify the benefits. And the benefits at this point are vague and not really substantiated scientifically."
According to the U.S. Centers for Disease Control and Prevention, 148 disease outbreaks tied to raw milk or raw milk products were reported in 1998 through 2011. Those caused 284 hospitalizations and two deaths.
"Contamination during milking or storage or milking from cows that may be diseased, exposes the consumer to severe and life-threatening illnesses such as miscarriage and still births in pregnant women, meningitis and blood infections in both young infants and pregnant women," Dr. Jatinder Bhatia told Reuters Health in an email.
Bhatia, from Children's Hospital of Georgia in Augusta, is one of the lead authors of the AAP statement.
In addition to babies and pregnant women, raw milk poses a health risk for people with compromised immune systems and the elderly, he said.
"The evidence overwhelmingly establishes the benefits of pasteurization on safety without proven adverse effects of pasteurization," Bhatia said.
The International Dairy Foods Association, a trade group, says on its website that "All milk intended for direct consumption should be pasteurized - it's a matter of food safety."
Boor grew up on a dairy farm and was raised on raw milk.
She said she favors giving people a choice when it comes to the type of milk they drink. But most people may not understand the risks of raw milk or accurately envision what goes on at a farm. Cows can be sick for a while before it's noticeable, Boor said, or the milking machine can drop off the cow and fall on the ground and get contaminated.
"Pasteurization is a very simple step, and that's all that it takes to put up that barrier, to prevent that problem," she said.What is meningitis? | ||
It's thought more than 1,500 people younger than 16 get the disease every year, and about one in 10 of those kids die.
Outbreaks of meningitis tend to make the news because they strike people who've been spending time together - at school or university for instance.
There are three types - A, B and C.
The risk of getting meningitis is very low. If you are feeling unwell, it's important to always tell your parents.
| ||
How do I know if I've got meningitis? | ||
One of the most common signs are tiny red or brown marks on the skin which can change colour.
Because getting a rash can mean many different things, there's a test to see if it may be to do with meningitis or not.
Press a glass against the rash - if the marks do not fade then this may be a rash from a form of meningitis.
As well as a rash, some of the other things you can feel with meningitis are:
| ||
Can meningitis be stopped? | ||
The only way to stop someone catching meningitis is by an injection called a vaccination which people get from doctors. Your body knows how to fight off some diseases like colds and coughs, but needs help to beat other ones. Vaccinations help people's bodies learn how to fight off other bugs and diseases. If you do know someone who has had meningitis, you don't need to avoid them. It is perfectly safe for you to play with someone who's had it and has recovered from it. | ||
What's being done about it? | ||
If an outbreak of the disease is spotted in a school, doctors are very quickly on the scene to make sure things are under control. They will make sure every pupil who needs it gets a vaccination.
The Meningitis Research Foundation is also doing more research to find out why young people seem to be affected more than others.
A website has been set up to help children and their parents learn more about what happens to people when they get meningitis and how to spot the signs and symptoms of the disease.
Viral meningitis refers to meningitis caused by a viral infection.[1] It is sometimes referred to as aseptic meningitis in contrast to meningitis caused by bacteria.
An example is lymphocytic choriomeningitis.
Viral meningitis is most commonly caused by enteroviruses.[2]
Causative organisms include:[1]
Treatment
Herpes simplex virus, varicella zoster virus and cytomegalovirus have a specific antiviral therapy; most other viruses do not. For HSV the treatment of choice is acyclovir.[3]
References
References
Sumber : Media online Kesehatan
| ||









I really appreciate DR AKHIGBE,my name is LAURIE HUGHES . I will never stop testifying DR AKHIGBE , Happiness is all i see now I never thought that I will be cured from HIV virus again. DR AKHIGBE did it for me I have been suffering from a deadly disease (HIV) for the past 2 years now, I had spent a lot of money going from one place to another, from churches to churches, hospitals have been my home every day residence. Constant checks up have been my hobby not until this faithful day, I saw a testimony on how DR AKHIGBE helped someone in curing his HIV disease in internet quickly I copied his email which is drrealakhigbe@gmail.com just to give him a test I spoke to him, he asked me to do some certain things which I did, he told me that he is going to provide the herbal cure to me, which he did, then he asked me to go for medical checkup after some days, after using the herbal cure and i did, behold I was free from the deadly disease,till now no HIV in me again he only asked me to post the testimony through the whole world, faithfully am doing it now,all the testimony of DR AKHIGBE is true please BROTHER and SISTER, MOTHER and FATHER he is great, I owe him in return. if you are having a similar problem just email him on drrealakhigbe@gmail.com or you can whats App his mobile number on +2348142454860 He can also cure these diseases like HIV and AIDS HERPES,DIABETICS,CANCER, HEPATITIS A&B,CHRONIC DISEASES, ASTHMA, HEART DISEASES, EXTERNAL INFECTION, EPILEPSY, STROKE, MULTIPLE SCLEROSIS, NAUSEA,VOMITING OR DIARRHEA,PARKINSON DISEASE,INFLUENZA,. COMMON COLD, AUTOIMMUNE DISORDER, MENINGITIS, LUPUS,ECZEMA,BACK PAIN, JOINT SCHIZOPHRENIA , PAIN.LOWER RESPIRATORY INFECTION. .ETC .please email drrealakhigbe@gmail.com or whats APP him ..+2348142454860 he is a real good and honest man.
BalasHapuswebsite... https:drrealakhigbe.weebly.com
I was diagnosed of Herpes 2 years ago and I have tried all possible means to get the cure but all to no avail, until I saw a post in a health forum about a Herbal Doctor(Dr Akhigbe) who prepares herbal medicine to cure all kind of diseases including Herpes, at first i doubted, if it was real but decided to give him a trial, when I contacted Dr Akhigbe through his Email: drrealakhigbe@gmail.com he guided me and prepared a herbal medicine and sent it to me via courier Delivery service,when I received the package (herbal medicine) He gave me instructions on how to consume it,I started using it as instructed and I stopped getting outbreaks and the sores started vanishing, could you believe I was cured of this deadly virus within two to three weeks and notices changes in my body. Days of using this REMEDY,couldn't believe the healing at first until I see it as my HERPES get cleared like magic Dr Akhigbe also use his herbal medicine to cure diseases like, HIV, HERPES, CANCER, ALS, CHRONIC DISEASE, HEART DISEASE, LUPUS, ASTHMA, DIABETES HEPATITIS A AND B.ECZEMA, BACK PAIN, EXTERNAL INFECTION ,ASTHMA, MENINGITIS, EPILEPSY,STROKE,KIDNEY DISEASE,ACME. etc Contact this great herbal Doctor today the father of herbal root cure. via Email: drrealakhigbe@gmail.com or whatsapp him +2348142454860 and get cured permanently He is real..website: https:drrealakhigbe.weebly.com
BalasHapusFor years, I have read and seen the advertisements in the mass media about all of the penis enhancement pills and thought that they were all scams or gimmicks. All of the medical sites that I have visited stated that none of the herbal supplements would ever help increase the size of a penis. I got very depressed when I read this, because unfortunately I was not naturally blessed with a penis that was big enough to arouse my sexual partner or past partners. I am a man that is past my sexual prime time and my sexual performance has a lot to be desired. I decided to try Doctor Akhigbe herbal medicine after all the reading and researching that I have done.I saw a testimony " Joe" about doctor Akhigbe Herbal Medicine Since there is a Money Back Guarantee, I give him a trial what did I have to lose? I couldn't believe the results I was seeing after drinking the Natural Herbal Medicine and Herbal Soap to be Rubin my penis! he sent to me through DHL courier delivery service . Within about 2 weeks I had a noticeable increase in the girth of my penis. Then after a couple of additional week it started to grow in length and I was amazed and very excited.before I finish the drink and the soap my penis had grown an additional two inches. I've had a considerable improvement with my sex life and these pills are certainly worth every penny I spent on them! I want to thank Dr Akhigbe for the time and effort they have spent on helping people in my situation.I know many are out there who are suffering this problem and they need help, email him. drrealakhigbe@gmail.com. He also cure other diseases like: Painful or Irregular Menstruation. HIV/Aids. Breast Enlargement. Diabetics. Vaginal Infections. Vaginal Discharge. Itching Of the Private Part. Breast Infection. Discharge from Breast. Breast Pain & Itching. Lower Abdominal Pain. No Periods or Periods Suddenly Stop. Women Sexual Problems. High Blood Pressure Chronic Disease. Pain during Sex inside the Pelvis. Pain during Urination. Pelvic Inflammatory Disease, (PID). Dripping Of Sperm from the Vagina As Well As for Low sperm count. Parkinson disease. Lupus. Cancer. Tuberculosis. Zero sperm count. Asthma. Quick Ejaculation. Corneal Ulcer, Gallstone, Terminal Illnesses, Premature Ejaculation. Herpes. Joint Pain. Stroke. Weak Erection. Erysipelas, Thyroid, Discharge from Penis. HPV. Impotence Effection, Hepatitis A and B. STD. Staphylococcus + Gonorrhea + Syphilis. Heart Disease. Pile-Hemorrhoid.rheumatism, thyroid, Autism, Penis enlargement, Waist & Back Pain. Male Infertility and Female Infertility. For your cure email him now: drrealakhigbe@gmail.com or Contact his number: +2349010754824.
BalasHapus