Perpustakaan keluarga :
Helmut Todo Tua Simamora dan dr. Olga Yanti V. Hutapea.
Berikut merupakan kutipan ilmiah kedokteran yang sangat bermanfaat sehingga disusun dan digunakan sebagai referensi pribadi.

What is blood pressure?

The direct answer to the question, "What is blood pressure?" is a short one:
Blood pressure is the force that moves blood through our circulatory system.
It is a life force because, without blood pressure, the following two basic provisions would not be pushed around our circulatory system to feed tissues and organs:1
- Oxygen
- Nutrients.
Blood pressure is vital also because it delivers white blood cells and antibodies for immunity, and hormones such as insulin.
Just as important as providing oxygen and nutrients, the fresh blood that gets delivered is able to pick up the toxic waste products of metabolism, including the carbon dioxide we exhale with every breath, and the toxins we clear through our liver and kidneys.
Blood itself carries a number of other properties, including its temperature. It also carries one of our defences against tissue damage, the clotting platelets that stem blood loss. See What is blood? for more information.
But what exactly is it that causes blood to exert a pressure in our arteries? Part of the answer is simple - the heart creates blood pressure by forcing out blood when it contracts with every heartbeat. Blood pressure, however, cannot be created solely by the pumping heart.
Biology and physics
Our circulation is a highly sophisticated form of plumbing - blood has 'flow' and arteries are 'pipes'. A basic law of physics gives rise to our blood flow, and it applies all the same in a garden hose pipe.
Blood flows through our body because of a difference in pressure - it has 'potential'.2 This is in the same sense of the word as used for another type of flow, that of electricity. 'Electrical potential', or voltage, forces an electrical current through a wire.
Our blood pressure is highest at the start of its journey from our heart - when it enters the aorta - and it is lowest at the end of its journey along progressively smaller branches of arteries. That pressure difference is what causes blood to flow around our bodies.
Just as the physical properties of a garden hose pipe affect the water pressure - constrict the pipe and the pressure is increased at that point - so too do arteries affect blood pressure.
Without the elastic nature of the artery walls, for example, the pressure of the blood would fall away more quickly as it is pumped from the heart.
So while the heart creates the maximum pressure, the properties of the arteries are just as important to maintaining it and allowing blood to flow throughout the body.
The condition of the arteries has effects on blood pressure and flow, and narrowing of the arteries can eventually block the supply altogether (a heart attack is the heart itself being cut off; a stroke is caused when arteries to the brain are blocked or bleed).
Measuring blood pressure
The way that blood pressure is measured today can be traced back to 18553 - the devices show how much pressure is needed before the pulse in our arm stops briefly: the arterial blood pressure is represented at that point.
The devices in use now still have a mouthful of a name - sphygmomamometer (from the Greek for pulse, sphygmo) - but you would recognize the typical rubber armband, the cuff that is inflated by hand or machine pump.
Once the cuff is inflated enough to stop the pulse, a reading is taken, either electronically or on an analogue dial.4
The reading is expressed in terms of the pressure it takes to move mercury round a tube against gravity in traditional scientific manometers - hence the unit, millimetres of mercury, that is abbreviated to mmHg.
The Mayo Clinic offers a video to show sphygmomamometry in action - it can be done by patients themselves, and modern blood pressure devices can also be used at home for people who need a more representative record of their blood pressure than the one given by a one-off clinic reading.
Systolic and diastolic readings
A stethoscope - another of those longstanding devices used by doctors - identifies the precise point when the pulse sound returns as the pressure of the cuff is slowly released. Using the stethoscope enables the person measuring the blood pressure to listen out for the two points at which to look at the gauge for the BP readings.
Medical dramas regularly have healthcare workers quoting two figures, with the systolic pressure first, 'over' the diastolic pressure - for example, '140 over 90.'Basically, the systolic pressure is the higher figure originated by the heart's contraction, while the diastolic one is the lower pressure in the arteries, during the brief 'resting' period between heartbeats.
What is normal blood pressure?
This is another question that doctors try to give a simple answer to, although blood pressure normality is complex.
Cardiologists do not really talk about a normal range - instead they work on the basis of when blood pressures should be considered too high, figures that continue to be refined by the medical research. The National Institutes of Health cites normal blood pressure to be below a certain level:5
- No greater than 120 mmHg systolic and 80 mmHg diastolic.
But blood pressure changes naturally, a fact that is best described in a quote from cardiologists writing about blood-pressure variability in a paper published by Nature in March 2013:6
"Blood pressure is characterized by marked short-term fluctuations occurring within a 24-hour period (beat-to-beat, minute-to-minute, hour-to-hour, and day-to-night changes) and also by long-term fluctuations occurring over more prolonged periods of time (days, weeks, months, seasons, and even years)."
The complexity of ambulatory (resting) blood pressure readings is witnessed by a 2013 review of the evolving international consensus. The paper - a 'brief review' - runs to some 4,000 words about measurement and the factors that influence it, including:7
- Measuring devices and software
- Number of readings
- White-coat hypertension (raised pressure because of anxiety about a reading)
- Nocturnal phenomena (night-time factors).
The guidelines followed by US doctors8 for the management of high blood pressure have been evolving too - but the general trend is that the threshold has been getting lower for when to start considering your blood pressure to be too high. This is most relevant to older people at greater risk of cardiovascular disease.
Perhaps the best clarity on what is considered a healthy, 'normal' blood pressure comes from knowing that keeping it from rising too much is all that really matters.
The guidelines8 state that for blood pressures above a figure of 115/75mmHg, every rise of 20/10mmHg doubles the risk of cardiovascular disease.
The overall hypertension guidelines received an update in December 2013,9 drawing from the evidence to recommend that anyone aged 60 years or more with hypertension should aim for a blood pressure level of less than 150/90mmHg.
Maintaining a healthy blood pressure level
The guidelines for doctors list the following measures patients can take to help keep a healthy blood pressure (from a table of evidence for the measures):8
- Keep a healthy body weight
- Eat a diet rich in fruits, vegetables, and low-fat dairy products
- Cut down on sodium intake (salt in the diet)
- Take regular aerobic exercise (eg, brisk walking) at least 30 minutes a day, most days of the week
- Moderate your alcohol drinking - keep under a maximum of 2 drinks a day for men and 1 drink a day for women/men of lighter weight (one drink having a half ounce of alcohol).
Arterial vasoconstriction is an important physiological process in regulating blood pressure, and is involved in pathologies. The isolation of arteries from rats and mice, as well as the measurement of vascular tension in an ex vivo preparation, are important methods in studying the physiology of arteries and the pathophysiology associated with arterials. Three major methods to measure vascular tension are organ bath, wire myograph, and pressurized arterial myograph. The major method to measure vascular remodeling is by observing the zero-stress state of an artery.
Arterial tone, one of the principal parameters of arterial function and regulation of blood pressure, is determined by the function of smooth muscle and the endothelium. Measuring contraction and relaxation in isolated arteries utilizes a range of methods that include organ bath as well as wire myography and pressurized diameter measurement system. This allows investigators to study physiological and pharmacological properties of arteries. Therefore, the ability to measure contraction and relaxation in isolated arteries is of great importance. Commonly used materials in tension experiments include strips, rings, and cannulated perfused vessels isolated from mouse and rat arteries. Preparations of isolated arteries enable one to study vascular function independent of systemic influences, which are present in in vivo preparations.
The most common animal models used for pulmonary hypertension are rats and mice with chronic hypoxia-induced pulmonary hypertension or monocrotaline-mediated pulmonary hypertension. It has to be noted, however, that differences of hemodynamics, histological (or structural) and functional changes in the pulmonary vasculature and right ventricle and pharmacological responses exist between patients with pulmonary hypertension and the animal models (rats and mice) of pulmonary hypertension.. Chronic hypoxia-induced pulmonary hypertension in mice, for example, causes minimal vascular remodeling, although pulmonary arterial pressure and pulmonary vascular resistance are both increased. In humans, however, pulmonary vascular remodeling, characterized by the intimal and medial thickening, is the major caused for the increased pulmonary vascular resistance [1]. In humans, adventitial thickening and fibrosis occur in the distal pulmonary arteries. However, in a study by Estrada and Chesler [2], a mouse model revealed that adventitial thickening and fibrosis occured in the proximal pulmonary arteries. In spite of this discrepancy, however, the use of chronically hypoxic rats and genetically modified mice will still provide significant insights into the pathogenic mechanisms of pulmonary hypertension that can be utilized to guide research for developing more effective and efficient therapeutic approaches for patients with pulmonary hypertension.
To facilitate future studies, we will describe methodologies for the isolation of pulmonary arteries from mice and rats, measurement of tension in isolated arteries, pharmacological modulation of contractility in isolated arteries, and other factors influencing contraction.
Isolation of pulmonary artery
Identifying the pulmonary artery for isolation
The rat and mouse lung consist of a single left lobe and four right lobes, which are called the cranial, medial, caudal, and postcaval lobes. Generally, the pulmonary artery is isolated from the left lobe due to the relative ease of working with a single, large lobe. The main pulmonary artery, originating from the right ventricle, splits into the left and right lobes of the lung. It then further splits into progressively smaller diameter vessels such as arterioles and capillaries as they extend to the end of lobe. It should be noted that, since the pulmonary artery and bronchial arteries run in parallel with one another, one should be careful to distinguish between the two. In general, the bronchial arterial wall consists of a thicker layer of smooth muscle cells compared to the pulmonary arterial wall. The isolated pulmonary artery from a mouse lung is shown in Figure 1A and the isolated pulmonary artery from a rat lung is shown in Figure 1B [3].

Figure 1
Image shows the isolated pulmonary artery. The pulmonary artery isolated from the left lobe in a 7–8 week old male, Balb C mouse; image from Nikon microscope (A). The pulmonary artery isolated from 8 week old male, SD rat; image from Nikon D-80 ...
Dissection and preparation of pulmonary arteries
The lung is removed from the chest cavity and washed with a physiological salt solution (PSS, pH 7.4) containing 138 mM NaCl, 4.7 mM KCl, 1.2 mM NH2PO4, 1.2 mM MgSO4, 1.8 mM CaCl2, 5 mM HEPES, and 10 mM glucose. The solution is oxygenated with 100% O2. The lung is positioned toward the ventral view and carefully stretched and pinned onto a dissecting dish, coated with a layer of silicone plastic (Sylgard), and placed under a light microscope. During the dissection, the PSS should be replaced frequently in the dissecting dish to allow for a better visualization of the arteries since lung tissues contain many air bubbles. When the superficial tissue of the lung is dissected away with fine micro-scissors, the bronchial artery is first seen lying above the pulmonary artery. Therefore, the bronchus artery needs to be carefully removed without damaging the pulmonary artery. The main pulmonary artery branches into left and right branches (extrapulmonary artery) which further branch into resistance arteries known as intrapulmonary arteries. They are named based on the order that they branch from the main pulmonary artery. Fourth or fifth order intralobar (intrapulmonary) branches (150-300 μm) for rats and second or third order branches (<200 μm) for mice are used in contraction experiments and carefully dissected away from connective tissues. The adventitia is carefully removed from isolated arteries under a high-magnification microscope. Extreme care should be taken to avoid stretching of the artery as it is detrimental to the experiment.
To mount the vessel as a ring preparation, the cleaned pulmonary artery should be cut into 1.5-2 mm ring segments. For the vascular strip preparation, helically cut the vascular wall in a spiral orientation. The vascular strip preparation has smooth muscle cells whose long axis is parallel to the strip so vascular contraction can develop more fully [4]. One must be careful that the orientation of the smooth muscle cells within the different strips be identical between vessels.
Cannulation of the vessel requires a segment length long enough to allow this. One should use vessel segments free of branches. However, this is often difficult as the pulmonary artery contains many branches. For that reason, this method is not commonly used by most investigators to measure resistance pulmonary arterial tone. More common methods include the use of an organ bath or wire myograph to measure isometric tension in isolated pulmonary arteries.
Arteries are composed of three layers. The inner layer (intima) is composed of single, flattened cells called endothelial cells, which cover the inner surface of the artery. In order to use endothelium-denuded arteries, it is necessary to carefully remove endothelium while avoiding damaging the smooth muscle cells. Removal of the endothelium from isolated vessels is generally accomplished by mechanical rubbing or air perfusion.
The vessel is cut open longitudinally so the endothelial layer at the intimal surface can be gently rubbed with a stainless steel wire. Alternatively, endothelial cells are disrupted by perfusing an air bolus through the lumen of the vessels. However, Liu et al. showed the loss of the myogenic response following removal of the endothelium via air perfusion [5]. Thus, air perfusion should not be used to evaluate the myogenic response. A successful removal of the arterial endothelium is verified functionally by the loss of the relaxation response to acetylcholine.
To study an endothelium-intact artery, one needs to prepare the pulmonary artery more carefully from connective tissue because the endothelium is easy to damage from the mechanical stretch induced during the process of isolation, mounting wire, or cannulation. To study endothelium-dependent relaxation, isolated pulmonary arteries are preconstricted with the contractile agonist, phenylephrine, typically at a concentration of 10−6 M. Cumulative relaxation curves of acetylcholine (10−9 to 10−5 M) are then constructed. Besides the pharmacological challenge to determine the presence of endothelium, histological staining can show intact endothelium and smooth muscle at the end of an experiment. In a previous study, it showed stained endothelial cells and smooth muscle cells using lectin and α-actin to show presence of endothelial cells from mouse pulmonary artery [6]. The pulmonary artery rings were fixed overnight in 10% neutral buffered formalin after contraction experiments. The vessel tissues were embedded in paraffin blocks in an automatic tissue processor (Sakura Tissue-Tek VIP; Sakura Finetek). The paraffin-embedded rings were serially sectioned at a thickness of 5 μm for staining with either lectin, for endothelium, or α-actin, for smooth muscle. The cells were visualized with a fluorescent microscope. The image confirmed that the vessel wall was preserved and had a distinct intraluminal wall composed of an endothelial cell monolayer (Figure 2A). Extracellular application of bradykinin, an endothelium-dependent vasodilator, significantly reduced active tension in pulmonary arterial rings pre-constricted with 40 mM K+ (Figure 2B and C).
Measurement of tension
Organ bath (ring or strip-mounted), wire (ring-mounted) myograph, and pressure myograph (pressurized vessel-mounted) are three common methods for studying functional responses and vascular reactivity in isolated arteries. In addition, the measurement of zero-stress in a pulmonary artery may be a useful tool to investigate the remodeling of the arterial wall. One should choose a particular method for studying vascular function based on the diameter of arteries, types of arteries, and purpose of experiments. Next, we will describe the technique of tension measurement and its application.
Organ bath
The organ bath system is a traditional method used to investigate the physiology and pharmacology of isolated vessels. Isotonic or isometric measurements can be made with appropriate transducers. An isometric measurement is most commonly used to measure vascular contractility as the vessel length remains constant.
In an isotonic measurement, the vessel length is shortened by force changes and is thus suitable to measure shortening velocities in vessels [7]. The organ bath, with isometric transducers, is commonly used to monitor tension in small tissue strips and rings (100 μm diameter) to large preparations.
Appropriate hooks or clips are selected depending on the diameter of the vessel. Ring segments are cut and two tungsten hooks are carefully passed through the lumen of pulmonary arterial rings in an organ bath containing PSS (Figure 3A). The bathing media is maintained at 37°C and is continuously aerated with 100% O2. One hook is attached to a displacement device, which allows the investigator to manually adjust the tension of the vessel, and the other hook is connected to an isometric force transducer [6]. The degree of adjustment of resting tension can affect vascular reactivity in response to a pharmacological agonist. Therefore, one needs to set the optimal resting tension. This is accomplished through a preliminary experiment to determine the maximum contraction induced by contractile agents such as high potassium chloride or norepinephrine. To set the optimal resting tension, the pulmonary arterial ring is stretched to different tensions and a contraction is elicited by pharmacological treatment at each tension. The tension which exhibits the largest contractile response is the optimal resting tension. In a previous study, the optimal resting (or basal) tension (300 mg) was determined, showing that active tension was significantly developed with exposure to the 40 mM K+ solution as the increasing the basal tension from 100 to 300 mg in isolated mouse pulmonary arterial rings [8]. For the rat pulmonary artery, the maximal tension developed the resting passive tension of 600-625 mg when the pulmonary arterial rings were exposed to the 40 mM K+ solution [9] with use of an isometric force transducer (Harvard Apparatus). Once at their optimal tension, the pulmonary arterial rings are allowed to further equilibrate for 30 minutes before the experiment. In all experiments, changes in the isometric force are measured with a force-displacement transducer connected to a carrier amplifier and then recorded on a pen recorder. After each experiment, the rings are weighed, and the active tension (mg) induced by agonists is normalized by wet tissue weight and expressed as milligram tension per milligram wet tissue weight (mg/mg).

Figure 3
A schematic diagram of a tension measurement. Organ chamber(A) and pressurized arterial myograph (B). The rabbit pulmonary artery was pressurized with 28 mmHg. ATP (10 μM) caused vasoconstriction in rabbit pulmonary artery.
Wire myograph
Wire myograph is a useful technique to examine vascular function and the reactivity of resistance arteries with an internal diameter as small as 60 μm, based on isometric tension recordings [10]. Ring preparations of small arteries with internal diameters between 100–500 μm can be mounted on 40 μm stainless steel wires. However, one should use 25 3m tungsten wires for arteries with an internal diameter around 60 3m (Danish Myotechnology). Two mounting wires are threaded through the isolated vessel lumen (ring preparation) and secured to two supports. One support is attached to a micrometer for the adjustment of vessel circumference and application of tension. The other support is attached to an isometric transducer. Following mounting and equilibration, the ring is normalized to an initial active wall tension. The normalization of wire-mounted arteries makes it important to set the preparation to an internal circumference that gives a maximal response and standardizes experiments. To determine the passive exponential wall tension-internal circumference (L) relationship, the artery is allowed to stretch at 1 minute intervals. The method involved calculation of an equivalent radial distending pressure from the measured arterial circumference and the radial force derived from the Laplace equation: Effective pressure=wall tension/internal radius. According to the normalization procedure in [11], the maximum force was developed when the vessel was set at 90% of the internal circumference it would achieve under an intraluminal pressure of 100 mmHg. The vessel set to L0, where L0= 0.9 × L100. In order to standardize the lumen diameter, the cross sectional area of the media of the mounted arteries (A) is calculated using the media thickness (m) and the circumference of vessels (L) based on the following equation: . Then, by using L0 and A, and assuming a constant media volume, the standardized media thickness of blood vessels (at L0) is calculated. The lumen diameter is defined as L0/π [12].
Pressurized arterial myograph
The pressurized arterial system allows the vessels to be closer to their in vivo condition and is used to study vascular function in physiology and patho-physiology states. It has been developed for use with resistant arteries (diameter >60 3m), and contractility is assessed by the changes in luminal diameter [13]. The isolated arteries are connected with perfusing cannulae which allow for the maintenance of intraluminal pressure that more closely models the physiology. The perfusing cannula (glass pipette) can be made to match the vessel lumen diameter using a model PP-83 vertical puller (Narishige, Tokyo, Japan). One cannula is in a fixed position while the other cannula is movable for the fine adjustment of longitudinal artery tension. Before the other side of artery is connected to the movable cannula, the artery is gently flushed to remove any blood and air bubbles from inside the vessel. All the side branches of pulmonary arteries are tied off using sutures to prevent leakage of intra-perfusing solution. A pressure transducer is used to maintain the appropriate pressure. In a previous report, they measured vessel diameter, pressurized to 12 mmHg, from the fourth order intrapulmonary artery of a rat with an inner diameter of 150 to 300 μm [14]. Outer flow in the bath chamber is maintained using a peristaltic pump. The temperature of the vessel environment is adjusted to 37°C and bubbled with oxygen. Internal lumen diameter and medial thickness of the vessel can be measured by a video camera attached to an imaging system (Figure 3B).
Zero-stress state of pulmonary artery
Vascular remodeling is mainly caused by excessive growth and proliferation of smooth muscle cells in the media and fibroblasts in the extracellular matrix, which also results in changes in the zero-stress state of the vessel. Therefore, to observe and measure changes in the zero-stress state is a valuable tool in determining vascular remodeling [15,16]. The zero-stress state is the stress-free configuration obtained by cutting vessel rings. When the rings are cut radially, the arterial wall will open at a specific angle [17]. The opening angle (θ) is the angle defined by two radii drawn from the midpoint of the inner wall to the tips of the inner wall of the open vessel ring. The physiological meaning of the opening angle can be defined as the residual strains in an artery at the no-load state and homeostatic strains at normal blood pressure [15]. Previous studies have demonstrated that the opening angle at the zero-stress state varies with non-uniform remodeling of the artery and arterial wall in hypertension, smoke exposure, diabetes, and aging [15,16,18-20]. Xu et al. compared pulmonary arterial rings (third- to fourth-order) isolated from left and right lungs with zero-stress state [6]. It was seen that left and right pulmonary arterial ring-shaped segments opened up into a sector (Figure 4). They found that the opening angles at the zero-stress states did not show a statistically significant difference between the left and right pulmonary artery. Conversely, the other study reported that the opening angles at the zero-stress states vary with the location and size of the pulmonary artery from a human [21].

Figure 4
Comparative residual angle or zero-stress state in pulmonary artery (PA) rings isolated from left and right lungs. At no-load state (top), the internal pressure, external pressure, and longitudinal stress in a short-ring-shaped segment of the left and ...
Vessel viability
After an equilibration period, it is necessary to test vascular contractibility and obtain a stable contractile response using various vasoconstrictors such as an increased concentration of potassium (NaCl replaced by KCl on a molar basis) or norepinephrine (10−6 M). This is done in order to have a baseline measurement of the viability of each individual artery so that one can later normalize experimental data as a percent of norepinephrine induced contraction, since the contractile responses may vary with vessel size and across species. Isolated vessels are considered viable if they contract more than 40% of their resting tone, in response to a contractile agent. If the artery does not contract appropriately, then either the optimal basal tension/lumen pressure has not been properly adjusted or the artery may have been damaged during isolation or mounting of the vessel.
Pharmacological characteristic of vascular tension
Endothelium-denuded vascular contraction
Contraction in vascular smooth muscle can be initiated by stretch/intraluminal pressure, membrane potential changes, or a pharmacological stimulus. Active force development can be caused by the passive stretch of smooth muscle and is called a myogenic response. A myogenic response keeps the vascular tension constant during an increase in intraluminal pressure [5].
Membrane depolarization of vascular smooth muscle cells can also elicit a contraction by activating voltage-dependent calcium channels (L-type calcium channels) in smooth muscle cells. This causes an increase of Ca2+ sensitivity on the contractile machinery or Ca2+ release from the sarcoplasmic reticulum [22,23]. For example, exposure of smooth muscle cells to high potassium causes membrane depolarization, thus stimulating Ca2+ influx though Ca2+ channels and resulting in contraction.
Regulation of vascular smooth muscle contraction can be modified by various pharmacological agents such as norepinepherine, angiotensin II, vasopressin, endothelin-1, serotonin, and thromboxane A2 6,24-28]. Each of these substances bind to their own receptors on the vascular smooth muscle cell or endothelium. These agents cause elevation in cytoplasmic calcium concentration through extracellular Ca2+ entry or Ca2+ release from intracellular stores, resulting in vascular contraction.
Endothelium-intact vascular contraction
Endothelial dysfunction is regarded as an early, key event in the development of vascular pathology [29]. A vital and quantifiable feature of endothelial dysfunction is the inability of vasodilation to occur in response to an appropriate stimulus, such as acetylcholine. The vascular endothelium releases endothelium-derived relaxing factors such as nitric oxide (NO), which promotes vascular relaxation by stimulating the production of guanylate cyclase and increasing the production of cGMP in smooth muscle, resulting in smooth muscle relaxation [30]. To evaluate NO viability, acetylcholine concentration-response curves are repeated after 30 minutes of incubation with the nitric oxide synthase inhibitor, N-nitro-L-arginine methyl ester (L-NAME, 10−4 M) [31], or the guanylyl cyclase inhibitor, 1H-[1, 2, 4]oxadiazolo[4, 3-alpha]quinoxalin-1-one (ODQ, 10−5 M) [32].
Factors influencing contractile activity
Many elements are important in improving the contractile vascular activity in one’s tension experiments. These elements include: 1) dissection skills, 2) optimal resting tension, 3) resistant artery, 4) age of animals, 5) buffer solution, 6) temperature of dissecting medium, and 7) isolation time (Table 1).
Table 1
Factors influencing contractile activity
The first methodological parameter to consider is a way to dissect the artery from its connective tissues. Proper care should be taken when using fine forceps to grasp only the connective tissue surrounding the vessel to avoid damaging and stretching the smooth muscle.
Secondly, the optimal resting tension must be determined accurately. Since the optimal resting tension depends on the vessel size, species, and type of artery, it should be determined before the experiment. The degree of initial preload applied to the vessel is the most critical factor in affecting vascular responses during the experiment. Regarding this aspect, previous studies have been reported that agonist-stimulated release of EDRF [33] and endothelium-dependent relaxation influenced by the initial stretch [34].
Thirdly, the size of isolated arteries is important because large conducting arteries contribute little to pulmonary vascular resistance. Resistance arteries should be isolated since they regulate pressure and flow. For instance, primary pulmonary hypertension occurs due to the constriction of small arteries, which then increases the resistance to blood flow through the lung [35]. Even though it is technically difficult to isolate resistance arteries, it is important to use them to study vascular function.
Next, the age of the animal can influence vascular function. It has been revealed that aging is associated with structural changes such as an increase in smooth muscle cell myofilament volume density [36]. In addition, the functional response of arteries can be affected by the age of animals. For example, the β adrenoceptor-mediated maximal relaxation has declined progressively as the age of the rats increased [37]. A previous report also suggested that the endothelium-mediated dilator response to acetylcholine was negligible at birth, but develops rapidly after birth, with a maximal effect at 3–10 days, and then declines gradually as one approaches adulthood. Also, it was observed that endothelium-independent dilator responses to sodium nitroprusside (SNP) were increased progressively with age in pulmonary artery [38]. Therefore, the age of the animals should be considered when designing experiments. In general, adult animals (7–8 weeks), weighing 300–500 grams for rats and 20–40 grams for mice, are used.
The fifth point to consider is the buffer solution chosen for the dissection and perfusing bath during the experiments as it affects the viability of the arteries. Alkalosis and acidosis, both, have a critical influence on pulmonary artery viability. Bicarbonate buffer is effective in buffering acids and bases, but it requires aeration with carbon dioxide (95% O2, 5% CO2) to maintain its pH. Alternatively, the artificial buffer, PSS, may be used as a buffer solution instead of bicarbonate solution by replacing the NaCO3 with HEPES, neutralized to pH 7.4 with NaOH, and aerated with 100% O2 [39]. For PSS, the pH should be adjusted at the experimental temperature because the pKa value of the artificial buffer is decreased with increases in temperature [40].
The sixth methodological parameter to consider is the temperature of the dissecting media. Low temperatures help to preserve the isolated tissue by slowing down degradation. Therefore, the dissection should be undertaken using chilled media (4°C).
Lastly, dissection and preparation of an isolated pulmonary artery should be undertaken as rapidly as possible.
Measurement of vascular contraction is an extremely useful tool for investigating physiological responses in normal conditions or abnormalities in pulmonary vascular disease. Several methods, with different scientific meanings and criteria for use, are available to measure vascular contraction and determine vascular remodeling. These methods include organ bath, wire myograph, pressurized artery myograph, and the zero-stress state of an artery. Pressurized artery myograph is more physiologically-based, but requires use of a non-branched pulmonary artery or, in the case of branches, the seal of all branches. When using the wire myograph technique, vessel leakage is not a concern. This review highlights the methodologies used for the preparation of the pulmonary artery and determination of its vascular function.
Blood pressure is a 'mathematical representation' of two forces. The top number (systolic) is the force applied against the walls of the arteries when the heart beats and the bottom number (diastolic) is the force applied against the walls between the two beats of the heart (i.e. when heart is in a relaxed state). A blood pressure range of 110/70 to 120/80 is considered normal.
Blood gas tension refers to the partial pressure of gases in blood.[1] There are several significant purposes for measuring gas tension;[2] the most common gas tensions measured are oxygen tension[3] (PxO2), the carbon dioxide tension[3] (PxCO2) and carbon monoxide tension[3] (PxCO). The subscript x in each symbol represents the source of the gas being measured; "a" meaning arterial,[3] "A" being alveolar,[3] "v" being venous,[3] "c" being capillary.[3] Blood gas tests (such asarterial blood gas tests) measure these partial pressures.
Oxygen tension
- Arterial blood oxygen tension (normal)
PaO2 — Partial pressure of oxygen at sea level (765 mmHg) in arterial blood is between 75 mmHg and 100 mmHg.[4][5][6]
- Venous blood oxygen tension (normal)
PvO2 — Oxygen tension in venous blood at sea level is between 30 mmHg and 40 mmHg.[6][7]
Carbon dioxide tension
Carbon dioxide is a by-product of food metabolism and in high amounts has toxic effects including: dyspnea, acidosis and altered consciousness.[8]
- Arterial blood carbon dioxide tension
PaCO2 — Partial pressure of carbon dioxide at sea level (765 mmHg) in arterial blood is between 35 mmHg and 45 mmHg.[9]
- Venous blood carbon dioxide tension
PvCO2 — Partial pressure of carbon dioxide at sea level in venous blood is between 40 mmHg and 50 mmHg.[9]
Carbon monoxide tension
- Arterial carbon monoxide tension (normal)
PaCO — Partial pressure of CO at sea level (765 mmHg) in arterial blood is approximately 0.02. It can be slightly higher in smokers and people living in dense urban areas.
Significance
The partial pressure of gas in blood is significant because it is directly related to ventilation and oxygenation.[10] When used alongside the pH balance of the blood, the PaCO2 and HCO3 (and Lactate) suggest to the health care practitioner which interventions, if any, should be made.[10][11] A survey of healthy individuals was done to measure the "normal" values of blood gas pressures and how it varies by age, sex, weight and height.[12] It was also found these values will depend on barometric pressure, and thus altitude. The predicted normal values of blood gas tensions and pH based on a patient's age, height, sex, and weight as well as the barometric pressure.
Equations
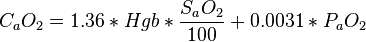
Oxygen content
The constant, 1.36, is the amount of oxygen (ml at 1 atmosphere) bound per gram of hemoglobin. The exact value of this constant varies from 1.34 to 1.39, depending on the reference and the way it is derived. The constant 0.0031 represents the amount of oxygen dissolved in plasma. The dissolved-oxygen term is generally small relative to the term for hemoglobin-bound oxygen, but becomes significant at very high PaO2 (as in a hyperbaric chamber) or in severe anemia.[13]
Oxygen saturation
This is an estimation and does not account for differences in temperature, pH and concentrations of 2,3 DPG.[14]
High blood pressure is also known as hypertension.Blood pressure is the amount of force exerted against the walls of the arteries as blood flows through them.
If a person has high blood pressure it means that the walls of the arteries are receiving too much pressure repeatedly - the pressure needs to be chronically elevated for a diagnosis of hypertension to be confirmed. In medicine chronic means for a sustained period; persistent.
High blood pressure statistics
In the USA approximately 72 million people have high blood pressure - about 1 in every 3 adults, according to the National Heart Lung and Blood Institute. The National Institutes of Health (NIH) estimates that about two-thirds of people over the age of 65 in the USA have high blood pressure.
In the UK, The National Health Service, estimates that about 40% of British adults have the condition.
In this article we will take you through what high blood pressure is, common causes, how it is diagnosed and the symptoms that often accompany it. We will also discuss the available treatments for high blood pressure and changes that you can make to help reduce your risk of suffering with high blood pressure.
Measuring blood pressure
The heart is a muscle that pumps blood around the body constantly - during every second of our lives. Blood that has low oxygen levels is pumped towards the lungs, where oxygen supplies are replenished. The oxygen rich blood is then pumped by the heart around the body to supply our muscles and cells. The pumping of blood creates pressure - blood pressure.
When we measure blood pressure, we gauge two types of pressure:
- Systolic pressure - the blood pressure when the heart contracts, specifically the moment of maximum force during the contraction. This happens when the left ventricle of the heart contracts.
- Diastolic pressure - the blood pressure between heartbeats, when the heart is resting and dilating (opening up, expanding).
When a person's blood pressure is taken the doctor or nurse needs to measure both the systolic and diastolic pressures. The figures usually appear with a larger number first (systolic pressure), followed by a smaller number (diastolic pressure). The figure will be followed by the abbreviation "mmHg", which means millimeters of mercury.
If you are told that your blood pressure is 120 over 80 (120/80 mmHg), it means a systolic pressure of 120mmHg and a diastolic pressure of 80mmHg.
What is high blood pressure?
Anyone whose blood pressure is 140/90mmhg or more for a sustained period is said to have high blood pressure, or hypertension.
Blood pressure is usually divided into five categories:
- Hypotension (low blood pressure)Systolic mmHg 90 or less, orDiastolic mmHg 60 or less
- NormalSystolic mmHg 90-119, andDiastolic mmHg 60-79
- PrehypertensionSystolic mmHg 120-139, andDiastolic mmHg 80-89
- Stage 1 HypertensionSystolic mmHg 140-159, andDiastolic mmHg 90-99
- Stage 2 HypertensionSystolic mmHg over 160, andDiastolic mmHg over 100
Symptoms of high blood pressure
Most people with high blood pressure will not experience any symptoms until levels reach about 180/110 mmHg.
High blood pressure symptoms typically include:
- Headache - usually, this will last for several days.
- Nausea - a sensation of unease and discomfort in the stomach with an urge to vomit.
- Vomiting - less common than just nausea.
- Dizziness - Lightheadedness, unsteadiness, and vertigo.
- Blurred or double vision (diplopia).
- Epistaxis - nosebleeds.
- Palpitations - disagreeable sensations of irregular and/or forceful beating of the heart.
- Dyspnea - breathlessness, shortness of breath.
Anybody who experiences these symptoms should see their doctor immediately.
Children with high blood pressure may have the following signs and symptoms:
- Headache.
- Fatigue.
- Blurred vision.
- Nosebleeds.
- Bell's palsy - inability to control facial muscles on one side of the face.
Newborns and very young babies with high blood pressure may experience the following signs and symptoms:
- Failure to thrive.
- Seizure.
- Irritability.
- Lethargy.
- Respiratory distress.
People who are diagnosed with high blood pressure should have their blood pressure checked frequently. Even if yours is normal, you should have it checked at least once every five years, and more often if you have any contributory factors.
On the next page we look at the causes of high blood pressure and how it is diagnosed. On the final page we examine the available treatments for high blood pressure, how lifestyle changes can help reduce blood pressure and the complications of high blood pressure.
Causes of high blood pressure
When referring to the causes of high blood pressure, it is divided into two categories:
- Essential high blood pressure (primary high blood pressure) - no cause has been identified.
- Secondary high blood pressure - the high blood pressure has an underlying cause, such as kidney disease, or a specific medication the patient is taking.
Even though there is no identifiable cause for essential high blood pressure, there is strong evidence linking some risk factors to the likelihood of developing the condition. Most of the causes below are essential high blood pressure risk factors; there are also a couple of secondary high blood pressure examples:
1) Age
The older you are the higher your risk of having high blood pressure.
2) Family history
If you have close family members with hypertension, your chances of developing it are significantly higher. An international scientific study involving over 150 scientists from 93 centers in Europe and the USA identified eight common genetic differences which may increase the risk of high blood pressure.
3) Temperature
A study which monitored 8801 participants over the age of 65 in three French cities, found that systolic and diastolic blood pressure values differed significantly across the four seasons of the year and according to the distribution of outdoor temperature. Blood pressure was lower when it got warmer, and rose when it got colder.
4) Ethnic background
Evidence in Europe and North America indicates that people with African and/or South Asian ancestry have a higher risk of developing hypertension, compared to people with predominantly Caucasian or Amerindian (indigenous of the Americas) ancestries.
5) Obesity/overweight
Overweight refers to having extra body weight from muscle, bone, fat and/or water. Obesity tends to refer just to having a high amount of extra body fat. Both overweight and obese people are more likely to develop high blood pressure, compared to people of normal weight.
6) Some aspects of gender
In general, high blood pressure is more common among adult men than adult women. However, after the age of 60 both men and women are equally susceptible. Women aged 18-59 are more likely to identify the signs and symptoms and subsequently to seek treatment for high blood pressure, compared to men.
7) Physical inactivity
Lack of exercise, as well as having a sedentary lifestyle, raises the risk of hypertension.
8) Smoking
Smoking causes the blood vessels to narrow, resulting in higher blood pressure. Smoking also reduces the blood's oxygen content so the heart has to pump faster in order to compensate, causing a rise in blood pressure.
9) Alcohol intake
The risk may even sometimes include people who drink regularly, but not in excess. People who drink regularly have higher systolic blood pressure than people who do not, said researchers from the University of Bristol, UK. They found that systolic blood pressure levels are about 7 mmHg higher in frequent drinkers than in people who do not drink.
10) High salt intake
Researchers from the University of Michigan Health System reported that societies where people don't eat much salt have lower blood pressures than places where people eat a lot of salt.
11) High fat diet
Many health professionals say that a diet high in fat leads to a raised high blood pressure risk. However, most dietitians stress that the problem is not how much fat is consumed, but rather what type of fats. Fats sourced from plants, such as avocados, nuts, olive oil, etc., as well as omega oils which are common in some types of fish, are good for you - while, saturated fats which are common in animal sourced foods, as well as trans fats are bad for you.
12) Mental stress
Various studies have offered compelling evidence that mental stress, especially over the long term, can have a serious impact on blood pressure. An interesting study carried out by researchers at the University of Texas, suggested that how air traffic controllers handle stress can affect whether they are at risk of developing high blood pressure later in life. In view of this study, and many others that focus on stress management, it seems fair to assume that some levels of stress which are not managed properly can raise the risk of hypertension.
13) Diabetes
People with diabetes are at a higher risk of developing hypertension. Among patients with diabetes type 1, hyperglycemia (high blood sugar) is a risk factor for incident hypertension in type 1 diabetes - intensive insulin therapy reduces the long-term risk of developing hypertension. People with diabetes type 2 are at risk of hypertension due to hyperglycemia, as well as other factors, such as overweight/obesity, certain medications, and some cardiovascular diseases.
14) Psoriasis
An American study that followed 78,000 women for 14 years found that having psoriasis was linked to a higher risk of developing high blood pressure and diabetes. Psoriasis is an immune system condition that appears on the skin in the form of thick, red scaly patches.
15) Pregnancy
Pregnant women have a higher risk of developing hypertension than women of the same age who are not pregnant. It is the most common medical problem encountered during pregnancy, complicating 2% to 3% of all pregnancies. Most countries divide hypertensive disorders in pregnancy into four categories: 1. Chronic hypertension, 2. Preeclampsia-eclampsia, 3. Preeclampsia superimposed on chronic hypertension. 4. Gestational hypertension.
Diagnosis of high blood pressure
Sphygmomanometer
Most lay people have seen this device. It consists of an inflatable cuff that is wrapped around the upper arm. When the cuff is inflated it restricts the blood flow. A mercury or mechanical manometer measures the pressure.
A sphygmomanometer is always used together with a means to determine at what pressure blood flow is just starting, and at what pressure it is unimpeded. For example, a manual sphygmomanometer is used together with a stethoscope.

- The cuff is placed snugly and smoothly around the upper arm, at approximately the same altitude as the heart while the patient is sitting up with the arm supported (resting on something). It is crucial that the size of the cuff is appropriate. If it is too small the reading will be inaccurately high; if it is too large the reading will be too low.
- The cuff is inflated until the artery is completely obstructed (occluded).
- The nurse, doctor, or whoever is doing the examination listens with a stethoscope to the brachial artery at the elbow and slowly releases the cuff's pressure (deflates it).
- As the cuffs pressure falls the examiner will hear a whooshing sound or a pounding sound when blood flow starts again.
- The pressure at the point when the sound began is noted down and recorded as the systolic blood pressure.
- The cuff is deflated further until no sound can be heard. At this point the examiner notes down and records the diastolic blood pressure.
With a digital sphygmomanometer everything is done with electrical sensors.
With advances in new wearable technology, people can now keep track of their blood pressure at home. You can read our review of the best home blood pressure monitors currently available to buy.
Confirmation of high blood pressure requires several readings
One blood pressure reading is not enough to diagnose hypertension in a patient. People's blood pressure can vary during the day, a visit to the doctor may spike the reading because the patient is anxious or stressed, having just eaten may also temporarily affect blood pressure readings.
As the definition of hypertension is defined as "repeatedly elevated blood pressure" the GP (general practitioner, primary care physician) will have to take several readings over a set period. This may require three separate measurements one week apart - often the monitoring goes on for much longer before a diagnosis is confirmed. On some rare occasions, if the blood pressure is extremely high, or end-organ damage is present, diagnosis may be made immediately so that treatment can start promptly. End-organ damage generally refers to damage to major organs fed by the circulatory system, such as the heart, kidneys, brain or eyes.
Kidney disorder - if the patient has a urinary tract infection, urinates frequently, or reports pain down the side of the abdomen, they could be signs/symptoms of a kidney disorder. If the doctor places the stethoscope on the side of the abdomen and hears the sound of a rush of blood (a bruit), it could be a sign of stenosis - a narrowing of an artery supplying the kidney.
Additional tests for high blood pressure
The doctor may also order the following tests to aid in diagnosis of high blood pressure:
- Urine and blood tests - underlying causes might be due to cholesterol, high potassium levels, blood sugar, infection, kidney malfunction, etc. Protein or blood in urine may indicate kidney damage. High glucose in the blood may indicate diabetes.
- Exercise stress test - more commonly used for patients with borderline hypertension. This usually involves pedaling a stationary bicycle or walking on a treadmill. The stress test assesses how the body's cardiovascular system responds to increased physical activity. If the patient has hypertension this data is important to know before the exercise test starts. The test monitors the electrical activity of the heart, as well as the patient's blood pressure during exercise. An exercise stress test sometimes reveals problems that are not apparent when the body is resting. Imaging scans of the heart's blood supply might be done at the same time.
- ECG (electrocardiogram) - this tests the heart's electrical activity. This test is more commonly used for patients at high risk of heart problems, such as hypertension and elevated cholesterol levels. The initial ECG is called a baseline. Subsequent ECGs may be compared with the baseline to reveal changes which may point to coronary artery disease or thickening of the heart wall.
- Holter monitoring - the patient carries an ECG portable device for about 24 hours.
- Echocardiogram - this device uses ultrasound waves which show the heart in motion. The doctor will be able to detect problems, such as thickening of the heart wall, defective heart valves, blood clots, and excessive fluid around the heart.
On the final page we look at the available treatments for high blood pressure, how lifestyle changes can help reduce blood pressure and the complications of high blood pressure.
Treatments for high blood pressure
Treatment for high blood pressure depends on several factors, such its severity, associated risks of developing stroke or cardiovascular, disease, etc.
Slightly elevated blood pressure
The doctor may suggest some lifestyle changes if the patient's blood pressure is only slightly elevated and the risk of developing cardiovascular disease considered to be small.
Moderately high blood pressure
If the patient's blood pressure is moderately high and the doctors believes the risk of developing cardiovascular disease during the next ten years is above 20%, the patient will probably be prescribed medication and advised on lifestyle changes.
Severe hypertension
If blood pressure levels are 180/110 mmHg or higher, the doctor will refer the patient to a specialist (cardiologist).
Changes in lifestyle can help lower high blood pressure
The following are recommended lifestyle changes that can help you lower your blood pressure. Note that you should always check with a Doctor or healthcare professional to discuss lifestyle changes before making any dramatic changes yourself.
Regular exercise

A regular program of exercise can prove beneficial in lowering blood pressure.
Exercising for 30 to 60 minutes five days a week will usually lower a person's blood pressure by 4 to 9 mmHg. If you embark on an exercise program you should see the benefits fairly soon - within a matter of two to three weeks, especially if you have been leading a sedentary lifestyle for a long time.
It is important to make sure you check with your doctor before embarking on any physical activity program. Exercise needs to be tailored to the needs and health of the patient.
The secret of getting success out of exercise is to do it regularly. Exercising at weekends and doing nothing from Monday to Friday will be much less effective.
Reducing alcohol consumption
Alcohol consumption is a double-edged sword. Some studies indicate it helps lower blood pressure, while others report the opposite. In very small amounts it may lower blood pressure. But if you drink too much, even moderate amounts regularly in some cases, blood pressure levels may go up. People who drink more than moderate amounts of alcohol regularly virtually always experience elevated blood pressure levels.
Eating healthily
This means eating plenty of fruits and vegetables, good quality unrefined carbohydrates, vegetable oils, and omega oils. If you eat animal products make sure all the fat is trimmed and avoid processed meats.
Lowering salt (sodium) intake
Studies have shown that even a moderate reduction in sodium intake can lower blood pressure levels by 2 to 8 mmHg.
A study found that most Americans who are diagnosed with hypertension still consume more than the recommended levels of salt. Study leader, Umed Ajani, an epidemiologist with the National Center for Chronic Disease Prevention and Promotion, said "Perhaps the most striking finding is that no difference in sodium intake was observed between those who received advice and those who did not."
A report published in March, 2009 by the Centers for Disease Control and Prevention (CDC), USA,suggests that 7 in every 10 adult Americans should limit their sodium intake to 1,500 mg a day(about 2/3 of a teaspoon of salt). The report estimated that 145 million Americans - 70% of the adult population - have one of three risk factors for hypertension.
Losing weight
Studies have revealed that even moderate weight loss - just ten pounds - can have a significant impact in lowering elevated blood pressure. If you are overweight, the nearer you get to your ideal weight the more your blood pressure is likely to fall. Any high blood pressure medications you are taking will become more effective when you lose weight. Reducing your waistline will have the greatest effect. Achieving your ideal body weight involves a combination of exercise, good diet, and at least 7 hours good quality sleep each night.
Keeping a food diary can double weight loss as part of a managed program, scientists at Kaiser Permanente's Center for Health Research discovered.
Lowering caffeine consumption
There are scores of studies that report on whether caffeine has an impact on blood pressure. As many of them have conflicting conclusions it is understandable that people become exasperated.
Habitual coffee drinking is not linked to an increased risk of high blood pressure in women, although a link was found with sugared or diet colas , reported researchers from Brigham and Women's Hospital and the Harvard School of Public Health.
Researchers found that healthy adults who drank two cans a day of a popular energy drink experienced an increase in their blood pressure and heart rate. The researchers, from Henry Ford Hospital believe the caffeine and taurine levels in energy drinks could be responsible for increases in blood pressure and heart rate.
All researchers agree on one thing: Excessive caffeine consumption is not good for people who have hypertension. Therefore, it would be wise to keep an eye on your caffeine consumption. Remember that caffeine is present in most coffees, many teas, sodas (carbonated drinks), chocolates, and some other foods and drinks.
Relaxation techniques
Researchers at Massachusetts General Hospital found that adding the relaxation response, a stress-management approach, to other lifestyle modifications may significantly improve treatment of the type of hypertension most common in the elderly.
Harvard Women's Health Watch reported that in one study, tai chi significantly boosted exercise capacity, lowered blood pressure, and improved levels of cholesterol, triglycerides, insulin, and C-reactive protein in people at high risk for heart disease.
Sleep
Not getting enough sleep can increase a person's risk of developing high blood pressure, scientists from the University of Chicago reported after monitoring over 500 middle aged people for 5 years.
Some studies have suggested that adults sleep no less than 7 hours and no more than 8 hours per day. In 2008 the American Academy of Sleep Medicine published a study suggesting that people with sleep duration above or below the recommended 7-to-8 hours per night face an increased risk of hypertension.
Recent developments on high blood pressure from MNT news
Could consuming probiotics help lower blood pressure?
We have all heard that consuming foods with probiotics - "good" bacteria - promotes a healthy gut. But new research published in the journal Hypertension suggests that eating probiotics could also help lower blood pressure.
Medications for treating high blood pressure
There are several anti-hypertensive medications on the market today. Some patients may need to take a combination of different drugs to effectively control their high blood pressure.
Some patients may have to be on medication to control hypertension for the rest of their lives. Doctors may advise discontinuing treatment if the patient has managed to maintain good blood pressure levels for a given period, and is not considered to be at significant risk of stroke or cardiovascular disease.
In a study, scientists from the Robarts Research Institute at The University of Western Ontario found that patients actually have more control of their high blood pressure when treated with less medication.
Below are some details of the most common drugs for treating high blood pressure:
1) Angiotensin-converting enzyme (ACE) inhibitors
ACE inhibitors block the actions of some hormones, such as angiotensin II, that regulate blood pressure. Angiotensin II causes the arteries to constrict, and increases blood volume, resulting in increased blood pressure. By inhibiting the actions of angiotensin II, the ACE inhibitors help reduce blood volume and also widen the arteries, both of which will cause the blood pressure drop.
People with a history of heart disease, pregnant women or individuals with conditions that affect the blood supply to the kidneys should not take ACE inhibitors.
Doctors may order a blood test to determine whether the patient has any pre-existing kidney problems. ACE inhibitors can reduce the blood supply to the kidneys, making them less efficient. Regular blood tests are usually carried out on patients taking ACE inhibitors.
ACE inhibitors may have the following more common side effects, which usually go away after a few days:
- Dizziness
- Fatigue
- Weakness
- Headaches
- Persistent dry cough (some people find the dry cough may continue)
Some patients may find the side effects too unpleasant or long-lasting. In such cases doctors will switch to an angiotensin-2 receptor antagonist. Side effects are less common, but may include dizziness, headache and/or hyperkalemia (elevated blood level of the electrolyte potassium).
Drug interaction - the effects of ACE inhibitors may be altered if taken with others medications, including some OTC (over-the-counter, non-prescription) drugs.
2) Calcium channel blockers
Calcium channel blockers (CCBs), among other things, decrease the calcium in blood vessels. A drop in calcium relaxes the vascular smooth muscle so that it does not contract so strongly, resulting in vasodilation (widening of arteries). If the arteries are wider blood pressure will drop.
Patients with a history of heart disease, liver disease, or problems with circulation should not take calcium channel blockers.
Calcium channel blockers may have the following more common side effects, which usually go away after a few days:
- Flushing - redness of the skin, usually over the cheeks or neck
- Headaches
- Edema (swelling) - swollen ankles, feet, and more rarely the abdomen
- Dizziness
- Fatigue
- Skin rash
Drug interaction - patients taking calcium channel blockers should avoid grapefruit.
3) Thiazide diuretics
Thiazide diuretics act on the kidneys to help the body eliminate sodium and water, resulting in less blood volume - less blood volume results in lower blood pressure. They are often the first choice in high blood pressure medications (but not the only choice).
Thiazide diuretics may cause the following side effects, some of which may persist:
- Hypokalemia - low blood potassium which can affect kidney and heart functions.
- Impaired glucose tolerance - raising risk of diabetes.
- Impotence (erectile dysfunction) - the side-effect resolves once the medication is withdrawn.
Patients taking thiazide diuretics should have regular blood and urine tests in order to monitor blood sugar and potassium levels.
Patients aged 80 or over may be given indapamide (Lozol), a special type of thiazide diuretic which helps reduce death from stroke, heart failure and some other cardiovascular diseases.
4) Beta-blockers
Beta-blockers were once very widely used for the treatment of hypertension. Because they have more potential side effects than other current hypertensive drugs, they tend to be used today when other treatments have not worked. Beta blockers slow the heart rate down, as well as reducing the force of the heart, resulting in a drop in blood pressure.
Beta blockers may have the following side effects:
- Fatigue.
- Cold hands and feet.
- Slow heartbeat.
- Nausea.
- Diarrhea.
- Disturbed sleep - beta-blockers decrease nocturnal melatonin release.
- Nightmares.
- Erectile dysfunction - difficulty in achieving or sustaining an erection.
The side effects below are also possible, but less common:
Drug interaction - the effects of beta-blockers may be altered if the patient takes some other medicines at the same time, causing adverse side-effects.
5) Renin inhibitors
Aliskiren (Tekturna, Rasilez) reduces renin production. Renin is an enzyme produced in the kidneys. Renin is involved in the production of a substance in the body called angiotensin I. Angiotensin I is converted into the hormone angiotensin II, which narrows blood vessels. Aliskiren blocks the production of angiotensin I so that levels of both angiotensin I and angiotensin II fall. This causes widening of the blood vessels, resulting in a drop in blood pressure. As it is a relatively new medication its use and dosages for patients with hypertension are still being determined.
Tekturna was approved in the US in March 2007 and in the European Union in August 2007 under the trade name Rasilez. Tekturna HCT, the first single-pill combination involving Tekturna, was approved in the US in January 2008. The single-pill combination Rasilez HCT was approved by the European Commission in January 2009. Rasilez is approved in over 70 countries.
Aliskiren may have the following side effects:
- Diarrhea
- Dizziness
- Flu-like symptoms
- Fatigue
- Cough
In February, 2009, the European Medicines Agency (EMEA) recommended adding a contra-indication to the Product Information for aliskiren, stating that it must not be used in patients who have experienced angioedema (swelling of the tissues beneath the skin).
Effectiveness of medications may vary according to patient's ethnicity
ACE inhibitors have been found to be more effective as a first choice medication in Caucasian patients, while calcium channel blockers or thiazide diuretics are generally more effective as a first choice medication for Afro-American and Afro-Caribbean patients, according to data from the USA and the UK.
If the above-mentioned medications, and their combinations are not effective
Some patients may still have trouble reaching desirable levels of blood pressure after being treated with the drugs mentioned so far. If this happens, the doctor may prescribe:
- Alpha blockers - they reduce the effects of natural chemicals that constrict (narrow) the blood vessels by reducing nerve impulses to the blood vessels.
- Alpha-beta blockers - they slow the heartbeat, which reduces the amount of blood pumping through the blood vessels, as well as reducing nerve impulses to the blood vessels.
- Central-acting agents - they stop the brain from telling the nervous system to raise the heart rate and constrict blood vessels.
In order to reduce the risk of cardiovascular disorder, some doctors may ask their patients to take dailyaspirin.
Complications of high blood pressure
If the hypertension is not treated or controlled the excessive pressure on the artery walls can lead to damage of the blood vessels (cardiovascular disease), as well as vital organs. The extent of damage depends on two factors; the severity of the hypertension and how long it goes on for untreated.
Below is a list of some of the possible complications of high blood pressure:
- Stroke - blood flow to the brain is impaired by blockage or rupture of an artery to the brain, and brain cells die.
- Heart attack - heart muscle dies due to a loss of blood supply.
- Heart failure - the heart struggles to pump enough blood to meet the needs of the whole body. This happens because after pumping blood against higher pressure into the blood vessels the heart muscle thickens.
- Blood clot - some blood converts from a liquid into a solid (thrombus). Some blood clots can cause serious complications.
- Aneurysm - a bulge forms on the wall of a vein, artery or the heart. The wall is weakened and may rupture.
- Kidney disease - hypertension often damages the small blood vessels in the kidneys, resulting in kidneys that do not work properly. Eventually the kidneys can fail completely (kidney failure).
- Eyes (hypertensive retinopathy) - untreated hypertension can lead to thickened, narrowed or torn blood vessels in the eyes, which can lead to vision loss.
- Metabolic syndrome - this is a disorder of the body's metabolism, including an enlarged waistline, low blood HDL levels (the good cholesterol), hypertension, and high levels of insulin. If the patient has hypertension he/she is more likely to have other components of metabolic syndrome, significantly raising the risk of diabetes, stroke and heart disease.
- Cognitive and memory problems - if the high blood pressure continues untreated the patient's ability to remember things, learn and understand concepts may be eventually become affected.
Sumber : Internet
http://www.medicalnewstoday.com/articles/270644.php#what_is_blood_pressure
http://www.ncbi.nlm.nih.gov/pmc/articles/PMC3501740/
http://www.medindia.net/patients/calculators/blood-pressure-calculator.asp
https://en.wikipedia.org/wiki/Blood_gas_tension

Tidak ada komentar:
Posting Komentar