Berikut merupakan kutipan ilmiah kesehatan yang bermanfaat sehingga disusun dan digunakan sebagai referensi pribadi.
Perpustakaan keluarga : Helmut Todo Tua Simamora dan dr. Olga Y.V Hutapea
What is Zika virus infection?
Zika virus infection is caused by the bite of an infected Aedes mosquito, usually causing mild fever, rash, conjunctivitis, and muscle pain.
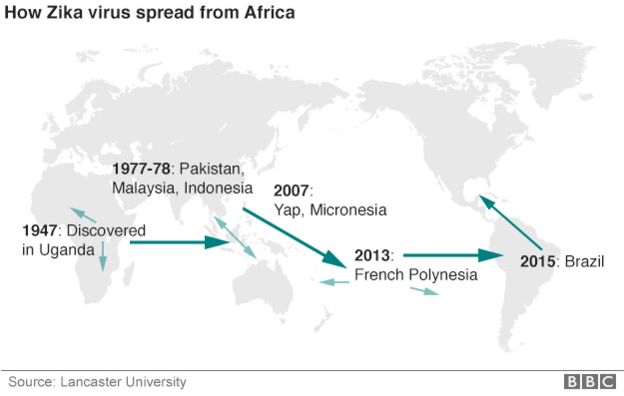
The virus was isolated for the first time in 1947 in the Zika forest in Uganda. Since then, it has remained mainly in Africa, with small and sporadic outbreaks in Asia. In 2007, a major epidemic was reported on the island of Yap (Micronesia), where nearly 75% of the population was infected.
On 3 March 2014, Chile notified PAHO/WHO that it had confirmed a case of indigenous transmission of Zika virus on Easter Island, where the virus continued to be detected until June 2014.
In May 2015, the public health authorities of Brazil confirmed the transmission of Zika virus in the northeast of the country. Since October 2015, other countries and territories of the Americas have reported the presence of the virus. See updated list at: www.paho.org/zikavirus.
What are the symptoms?
The most common symptoms of Zika virus infection are mild fever and exanthema (skin rash), usually accompanied by conjunctivitis, muscle or joint pain, and general malaise that begins 2-7 days after the bite of an infected mosquito.
One out of four infected people develops symptoms of the disease. Among those who do, the disease is usually mild and can last 2-7 days. Symptoms are similar to those of dengue or chikungunya, which are transmitted by the same type of mosquito. Neurological and autoimmune complications are infrequent, but have been described in the outbreaks in Polynesia and, more recently, in Brazil. As the virus spreads in the Americas, giving us more experience with its symptoms and complications, it will be possible to characterize the disease better.
How is Zika virus transmitted?
Zika virus is transmitted to people through the bite of an infected Aedes mosquito. This is the same mosquito that transmits dengue and chikungunya.
Can it be transmitted through blood or sexual contact?
In general, the Zika virus needs a vector (a means of transportation) to infect people. That vector is the mosquito. The virus has also been isolated in semen, and one case of possible person-to-person sexual transmission has been described, but not confirmed.
Zika can be transmitted through blood, but this is an infrequent mechanism. The usual recommendations for safe transfusions should be followed (e.g., healthy volunteer donors).
Can it be transmitted from mother to child?
There is little information on transmission from mother to baby during pregnancy or childbirth. Perinatal transmission has been reported with other vector-borne viruses, such as dengue and chikungunya. Studies are now being conducted on possible mother-to-child transmission of the virus and its possible effects on the baby. More information.
What treatment is there?
Treatment consists of relieving pain, fever, and any other symptom that inconveniences the patient. To prevent dehydration, it is recommended to control the fever, rest, and drink plenty of water. There is no vaccine or specific drug for this virus.
Can it cause death?
In this Region, it is a new virus that up until now has had a very limited geographical and demographic distribution, and there is no evidence that it can cause death. However, sporadic cases have been reported of more serious manifestations and complications in patients with preexisting diseases or conditions, causing death.
Who is at risk of Zika infection?
Anyone not previously exposed to the virus and who lives in an area where the mosquito is present, and where imported or local cases have been reported, may be infected. Since the Aedes mosquito is found throughout the Region (except in continental Chile and Canada), it is likely that outbreaks will occur in other countries that have not yet reported any cases.
How is Zika diagnosed?
In most people, diagnosis is based on clinical symptoms and epidemiological circumstances (such as Zika outbreak in the patient’s area or trips to areas where the virus is circulating).
Blood tests can help to confirm the diagnosis. Some (virological PCR tests) are useful in the first 3-5 days after the onset of symptoms, while others (serological tests) detect the presence of antibodies but are useful only after five days.
Once it has been demonstrated that the virus is present in a given area or territory, confirmation of all cases is not necessary, and laboratory testing will be adjusted to routine virological surveillance of the disease.
Which is the difference between Zika, dengue, and chikungunya?
All these diseases present similar symptoms, but certain symptoms suggest one disease or another:
Dengue usually presents with higher fever and more severe muscle pain. There can be complications when the fever breaks: attention should be paid to warning signs such as bleeding.
Chikungunya presents with higher fever and more intense joint pain, affecting the hands, feet, knees, and back. It can disable people, bending them over so that they cannot walk or perform simple actions such as opening a water bottle.
Zika does not have clearly characteristic features, but most patients have skin rashes and some have conjunctivitis.
Is there a relationship between Guillain-Barré syndrome and Zika virus?
An increase in Guillain-Barré syndrome (GBS) has been observed in areas where a Zika virus epidemic has been documented (e.g., in French Polynesia and Brazil).
However, a direct causal relationship has not been established between Zika virus infection and GBS. Prior infection with dengue or genetic factors could contribute to or increase cases of GBS. Several studies are underway to better establish the relationship between Zika and GBS.
GBS occurs when a person’s immune system attacks itself, in particular affecting the cells of the nervous system. This process can be initiated by infection with various viruses or bacteria. The main symptoms include muscular weakness and tingling (paresthesia) in the arms and legs, and severe complications can occur if the respiratory muscles are affected. The most seriously ill patients need attention in intensive care units.
CIRCULATION OF ZIKA VIRUS
Which countries have reported cases of Zika in the Americas?
On 3 March 2014, Chile notified PAHO/WHO that it had confirmed a case of indigenous transmission of Zika virus on Easter Island, where the virus continued to be detected until June 2014.
In May 2015, the public health authorities of Brazil confirmed the transmission of Zika virus in the northeast of the country. Since October 2015, other countries and territories of the Americas have reported the presence of the virus. (See updated list at: www.paho.org/zikavirus.
What causes rapid transmission in an area?
There are two factors for rapid transmission (documented in other countries): (1) Since this is a new virus to the Americas, the entire population is susceptible, lacking defenses to Zika virus; and (2) The Aedes mosquito is widespread in the Region, given the climatic conditions, temperature, and humidity in tropical countries.
Is it advisable to travel to countries where Zika virus is circulating?
PAHO/WHO does not recommend any travel or international trade restrictions related to Zika virus outbreaks. Travelers are advised to take the suggested precautions to prevent mosquito bites.
How many Zika cases have been reported in the Region of the Americas?
Countries begin reporting when they detect the circulation of the virus in their territories. However, maintaining a case count is difficult because symptoms of the disease tend to be mild and not everyone affected is seen by health services. What is most important is to detect the circulation of the virus, strengthen the response of health services, and step up surveillance of serious cases and complications.
PREVENTION
What measures should be taken to prevent Zika virus infection?
Prevention involves reducing mosquito populations and avoiding bites, which occur mainly during the day. Eliminating and controlling Aedes aegypti mosquito breeding sites reduces the chances that Zika, chikungunya, and dengue will be transmitted. An integrated response is required, involving action in several areas, including health, education, and the environment.
To eliminate and control the mosquito, it is recommended to:
- Avoid allowing standing water in outdoor containers (flower pots, bottles, and containers that collect water) so that they do not become mosquito breeding sites.
- Cover domestic water tanks so that mosquitoes cannot get in.
- Avoid accumulating garbage: Put it in closed plastic bags and keep it in closed containers.
- Unblock drains that could accumulate standing water.
- Use screens and mosquito nets in windows and doors to reduce contact between mosquitoes and people.
To prevent mosquito bites, it is recommended that people who live in areas where there are cases of the disease, as well as travelers and, especially, pregnant women should:
- Cover exposed skin with long-sleeved shirts, trousers, and hats
- Use repellents recommended by the health authorities (and apply them as indicated on the label)
- Sleep under mosquito nets.
People with symptoms of Zika, dengue, or chikungunya should visit a health center.
What is PAHO/WHO’s response in the Americas?
PAHO/WHO is working actively with the countries of the Americas to develop or maintain their ability to detect and confirm cases of Zika virus infection, treat people affected by the disease, and implement effective strategies to reduce the presence of the mosquito and minimize the likelihood of an outbreak. PAHO/WHO’s support involves:
- Building the capacity of laboratories to detect the virus in a timely fashion (together with other collaborating centers and strategic partners).
- Advising on risk communication to respond to the introduction of the virus in the country.
- Controlling the vector by working actively with the populace to eliminate mosquito populations.
- Preparing recommendations for the clinical care and monitoring of persons with Zika virus infection, in collaboration with professional associations and experts from the countries.
- Monitoring the geographic expansion of the virus and the emergence of complications and serious cases through surveillance of events and country reporting through the International Health Regulations channel.
- Supporting health ministry initiatives aimed at learning more about the characteristics of the virus, its impact on health, and the possible consequences of infection.
- Zika virus disease is caused by a virus transmitted by Aedes mosquitoes.
- People with Zika virus disease usually have a mild fever, skin rash (exanthema) and conjunctivitis. These symptoms normally last for 2-7 days.
- There is no specific treatment or vaccine currently available.
- The best form of prevention is protection against mosquito bites.
- The virus is known to circulate in Africa, the Americas, Asia and the Pacific.
PAHO/WHO is working actively with the countries of the Americas to develop or maintain their ability to detect and confirm cases of Zika virus infection, treat people affected by the disease, and implement effective strategies to reduce the presence of the mosquito and minimize the likelihood of an outbreak. PAHO/WHO’s support involves:
- Building the capacity of laboratories to detect the virus in a timely fashion (together with other collaborating centers and strategic partners).
- Advising on risk communication to respond to the introduction of the virus in the country.
- Controlling the vector by working actively with the populace to eliminate mosquito populations.
- Preparing recommendations for the clinical care and monitoring of persons with Zika virus infection, in collaboration with professional associations and experts from the countries.
- Monitoring the geographic expansion of the virus and the emergence of complications and serious cases through surveillance of events and country reporting through the International Health Regulations channel.
- Supporting health ministry initiatives aimed at learning more about the characteristics of the virus, its impact on health, and the possible consequences of infection.
Introduction
Zika virus is an emerging mosquito-borne virus that was first identified in Uganda in 1947 in rhesus monkeys through a monitoring network of sylvatic yellow fever. It was subsequently identified in humans in 1952 in Uganda and the United Republic of Tanzania. Outbreaks of Zika virus disease have been recorded in Africa, the Americas, Asia and the Pacific.
- Genre: Flavivirus
- Vector: Aedes mosquitoes (which usually bite during the morning and late afternoon/evening hours)
- Reservoir: Unknown
Zika virus is an emerging mosquito-borne virus that was first identified in Uganda in 1947 in rhesus monkeys through a monitoring network of sylvatic yellow fever. It was subsequently identified in humans in 1952 in Uganda and the United Republic of Tanzania. Outbreaks of Zika virus disease have been recorded in Africa, the Americas, Asia and the Pacific.
- Genre: Flavivirus
- Vector: Aedes mosquitoes (which usually bite during the morning and late afternoon/evening hours)
- Reservoir: Unknown
Signs and Symptoms
The incubation period (the time from exposure to symptoms) of Zika virus disease is not clear, but is likely to be a few days. The symptoms are similar to other arbovirus infections such as dengue, and include fever, skin rashes, conjunctivitis, muscle and joint pain, malaise, and headache. These symptoms are usually mild and last for 2-7 days.
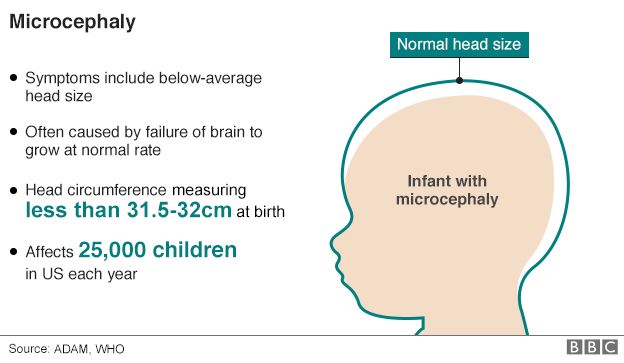
During large outbreaks in French Polynesia and Brazil in 2013 and 2015 respectively, national health authorities reported potential neurological and auto-immune complications of Zika virus disease. Recently in Brazil, local health authorities have observed an increase in Zika virus infections in the general public as well as an increase in babies born with microcephaly in northeast Brazil. Agencies investigating the Zika outbreaks are finding an increasing body of evidence about the link between Zika virus and microcephaly. However, more investigation is needed before we understand the relationship between microcephaly in babies and the Zika virus. Other potential causes are also being investigated.
The incubation period (the time from exposure to symptoms) of Zika virus disease is not clear, but is likely to be a few days. The symptoms are similar to other arbovirus infections such as dengue, and include fever, skin rashes, conjunctivitis, muscle and joint pain, malaise, and headache. These symptoms are usually mild and last for 2-7 days.
During large outbreaks in French Polynesia and Brazil in 2013 and 2015 respectively, national health authorities reported potential neurological and auto-immune complications of Zika virus disease. Recently in Brazil, local health authorities have observed an increase in Zika virus infections in the general public as well as an increase in babies born with microcephaly in northeast Brazil. Agencies investigating the Zika outbreaks are finding an increasing body of evidence about the link between Zika virus and microcephaly. However, more investigation is needed before we understand the relationship between microcephaly in babies and the Zika virus. Other potential causes are also being investigated.
Transmission
Zika virus is transmitted to people through the bite of an infected mosquito from the Aedes genus, mainly Aedes aegypti in tropical regions. This is the same mosquito that transmits dengue, chikungunya and yellow fever.
Zika virus disease outbreaks were reported for the first time from the Pacific in 2007 and 2013 (Yap and French Polynesia, respectively), and in 2015 from the Americas (Brazil and Colombia) and Africa (Cape Verde). In addition, more than 13 countries in the Americas have reported sporadic Zika virus infections indicating rapid geographic expansion of Zika virus.
Zika virus is transmitted to people through the bite of an infected mosquito from the Aedes genus, mainly Aedes aegypti in tropical regions. This is the same mosquito that transmits dengue, chikungunya and yellow fever.
Zika virus disease outbreaks were reported for the first time from the Pacific in 2007 and 2013 (Yap and French Polynesia, respectively), and in 2015 from the Americas (Brazil and Colombia) and Africa (Cape Verde). In addition, more than 13 countries in the Americas have reported sporadic Zika virus infections indicating rapid geographic expansion of Zika virus.
Diagnosis
Zika virus is diagnosed through PCR (polymerase chain reaction) and virus isolation from blood samples. Diagnosis by serology can be difficult as the virus can cross-react with other flaviviruses such as dengue, West Nile and yellow fever.
Zika virus is diagnosed through PCR (polymerase chain reaction) and virus isolation from blood samples. Diagnosis by serology can be difficult as the virus can cross-react with other flaviviruses such as dengue, West Nile and yellow fever.
Prevention
Mosquitoes and their breeding sites pose a significant risk factor for Zika virus infection. Prevention and control relies on reducing mosquitoes through source reduction (removal and modification of breeding sites) and reducing contact between mosquitoes and people.
This can be done by using insect repellent; wearing clothes (preferably light-coloured) that cover as much of the body as possible; using physical barriers such as screens, closed doors and windows; and sleeping under mosquito nets. It is also important to empty, clean or cover containers that can hold water such as buckets, flower pots or tyres, so that places where mosquitoes can breed are removed.
Special attention and help should be given to those who may not be able to protect themselves adequately, such as young children, the sick or elderly.
During outbreaks, health authorities may advise that spraying of insecticides be carried out. Insecticides recommended by the WHO Pesticide Evaluation Scheme may also be used as larvicides to treat relatively large water containers.
Travellers should take the basic precautions described above to protect themselves from mosquito bites.
Mosquitoes and their breeding sites pose a significant risk factor for Zika virus infection. Prevention and control relies on reducing mosquitoes through source reduction (removal and modification of breeding sites) and reducing contact between mosquitoes and people.
This can be done by using insect repellent; wearing clothes (preferably light-coloured) that cover as much of the body as possible; using physical barriers such as screens, closed doors and windows; and sleeping under mosquito nets. It is also important to empty, clean or cover containers that can hold water such as buckets, flower pots or tyres, so that places where mosquitoes can breed are removed.
Special attention and help should be given to those who may not be able to protect themselves adequately, such as young children, the sick or elderly.
During outbreaks, health authorities may advise that spraying of insecticides be carried out. Insecticides recommended by the WHO Pesticide Evaluation Scheme may also be used as larvicides to treat relatively large water containers.
Travellers should take the basic precautions described above to protect themselves from mosquito bites.
Treatment
Zika virus disease is usually relatively mild and requires no specific treatment. People sick with Zika virus should get plenty of rest, drink enough fluids, and treat pain and fever with common medicines. If symptoms worsen, they should seek medical care and advice. There is currently no vaccine available.
Zika virus disease is usually relatively mild and requires no specific treatment. People sick with Zika virus should get plenty of rest, drink enough fluids, and treat pain and fever with common medicines. If symptoms worsen, they should seek medical care and advice. There is currently no vaccine available.
WHO Response
WHO is supporting countries to control Zika virus disease through:
- strengthening surveillance;
- building the capacity of laboratories to detect the virus;
- working with countries to eliminate mosquito populations;
- preparing recommendations for the clinical care and monitoring of persons with Zika virus infection; and
- defining and supporting priority areas of research into Zika virus disease and possible complications.
What is the Zika virus:
WHO is supporting countries to control Zika virus disease through:
- strengthening surveillance;
- building the capacity of laboratories to detect the virus;
- working with countries to eliminate mosquito populations;
- preparing recommendations for the clinical care and monitoring of persons with Zika virus infection; and
- defining and supporting priority areas of research into Zika virus disease and possible complications.
What is the Zika virus:
- Spread by the Aedes aegyptimosquito, which also carries dengue fever and yellow fever
- First discovered in Africa in the 1940s but is now spreading in Latin America
- Scientists say there is growing evidence of a link to microcephaly, that leads to babies being born with small heads
- Can lead to fever and a rash but most people show no symptoms, and there is no known cure
- Only way to fight Zika is to clear stagnant water where mosquitoes breed, and protect against mosquito bites

US scientists have urged the World Health Organisation to take urgent action over the Zika virus, which they say has "explosive pandemic potential".
Writing in a US medical journal, they called on the WHO to heed lessons from the Ebola outbreak and convene an emergency committee of disease experts.
They said a vaccine might be ready for testing in two years but it could be a decade before it is publicly available.
Zika, linked to shrunken brains in children, has caused panic in Brazil.
Thousands of people have been infected there and it has spread to some 20 countries.
The Brazilian President, Dilma Roussef, has urged Latin America to unite in combating the virus.
She told a summit in Ecuador that sharing knowledge about the disease was the only way that it would be beaten. A meeting of regional health ministers has been called for next week.
Writing in the Journal of the American Medical Association, Daniel R Lucey and Lawrence O Gostin say the WHO's failure to act early in the recent Ebola crisis probably cost thousands of lives.
They warn that a similar catastrophe could unfold if swift action is not taken over the Zika virus.
"An Emergency Committee should be convened urgently to advise the Director-General about the conditions necessary to declare a Public Health Emergency of International Concern," Mr Lucey and Mr Gostin wrote.
They added: "The very process of convening the committee would catalyze international attention, funding, and research."
White House spokesman Josh Earnest said on Wednesday the US government intended to make a more concerted effort to communicate with Americans about the risks associated with the virus.
No cure
There is no cure for the virus and the hunt is on for a vaccine, led by scientists at the University of Texas Medical Branch.
The researchers have visited Brazil to carry out research and collect samples and are now analysing them in a suite of high-security laboratories in Galveston, Texas.
Access to the building in Galveston is tightly controlled by police and the FBI. Speaking to the BBC inside the facility, Professor Scott Weaver, director of the Institute for Human Infections and Immunity, said people were right to be frightened by the virus.
"It's certainly a very significant risk," he said, "and if infection of the foetus does occur and microcephaly develops we have no ability to alter the outcome of that very bad disease which is sometimes fatal or leaves children mentally incapacitated for the remainder of their life."
The Zika virus was discovered in monkeys in 1947 in Uganda's Zika Forest, with the first human case registered in Nigeria in 1954 but for decades it did not appear to pose much of a threat to people and was largely ignored by the scientific community.
It was only with an outbreak on the Micronesian island of Yap in 2007 that some researchers began to take an interest.
In the past year the virus "exploded" said Prof Weaver, sweeping through the Caribbean and Latin America "infecting probably a couple of million people".
The symptoms in adults and children are similar to those for dengue fever but generally milder, including flu-like aches, inflammation of the eyes, joint pain and rashes although some people have no symptoms at all.
In rare cases the disease may also lead to complications including Guillain-Barre syndrome, a disorder of the nervous system which can cause paralysis.
Symptoms
- About 1 in 5 people infected with Zika virus become ill (i.e., develop Zika).
- The most common symptoms of Zika are fever, rash, joint pain, or conjunctivitis (red eyes). Other common symptoms include muscle pain and headache. The incubation period (the time from exposure to symptoms) for Zika virus disease is not known, but is likely to be a few days to a week.
- The illness is usually mild with symptoms lasting for several days to a week.
- Zika virus usually remains in the blood of an infected person for a few days but it can be found longer in some people.
- Severe disease requiring hospitalization is uncommon.
- Deaths are rare.
Diagnosis
- The symptoms of Zika are similar to those of dengue and chikungunya, diseases spread through the same mosquitoes that transmit Zika.
- See your healthcare provider if you develop the symptoms described above and have visited an area where Zika is found.
- If you have recently traveled, tell your healthcare provider when and where you traveled.
- Your healthcare provider may order blood tests to look for Zika or other similar viruses like dengue or chikungunya.
Treatment
- No vaccine or medications are available to prevent or treat Zika infections.
- Treat the symptoms:
- Get plenty of rest
- Drink fluids to prevent dehydration
- Take medicines, such as acetaminophen or paracetamol, to relieve fever and pain
- Do not take aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs), like ibuprofen and naproxen. Aspirin and NSAIDs should be avoided until dengue can be ruled out to reduce the risk of hemorrhage (bleeding). If you are taking medicine for another medical condition, talk to your healthcare provider before taking additional medication.
- If you have Zika, avoid mosquito bites for the first week of your illness.
- During the first week of infection, Zika virus can be found in the blood and passed from an infected person to another mosquito through mosquito bites.
- An infected mosquito can then spread the virus to other people.
Modes of Transmission
Zika virus is a single-stranded RNA virus of the Flaviviridae family, genus Flavivirus. Zika virus is transmitted to humans primarily through the bite of an infected Aedes species mosquito. The mosquito vectors typically breed in domestic water-holding containers; they are aggressive daytime biters and feed both indoors and outdoors near dwellings. Nonhuman and human primates are likely the main reservoirs of the virus, and anthroponotic (human-to-vector-to-human) transmission occurs during outbreaks.
Perinatal, in utero, and possible sexual and transfusion transmission events have also been reported. Zika virus RNA has been identified in asymptomatic blood donors during an ongoing outbreak.
Clinical Signs & Symptoms
About 1 in 5 people infected with Zika virus become symptomatic. Characteristic clinical findings are acute onset of fever with maculopapular rash, arthralgia, or conjunctivitis. Other commonly reported symptoms include myalgia and headache. Clinical illness is usually mild with symptoms lasting for several days to a week. Severe disease requiring hospitalization is uncommon and case fatality is low. However, there have been cases of Guillain-Barre syndrome reported in patients following suspected Zika virus infection. The Brazil Ministry of Health is also investigating the possible association between Zika virus and a reported increase in the number of babies born with microcephaly. Due to concerns of microcephaly associated with maternal Zika virus infection, fetuses and infants of women infected with Zika virus during pregnancy should be evaluated for possible congenital infection and neurologic abnormalities.
Diagnosis & Reporting
Based on the typical clinical features, the differential diagnosis for Zika virus infection is broad. In addition to dengue, other considerations include leptospirosis, malaria, rickettsia, group A streptococcus, rubella, measles, and parvovirus, enterovirus, adenovirus, and alphavirus infections (e.g., Chikungunya, Mayaro, Ross River, Barmah Forest, O’nyong-nyong, and Sindbis viruses).
Preliminary diagnosis is based on the patient’s clinical features, places and dates of travel, and activities. Laboratory diagnosis is generally accomplished by testing serum or plasma to detect virus, viral nucleic acid, or virus-specific immunoglobulin M and neutralizing antibodies. Click for more information about diagnostic testing.
In 2016, Zika virus disease became a nationally notifiable condition. Healthcare providers are encouraged to report suspected cases to their state or local health departments to facilitate diagnosis and mitigate the risk of local transmission. State health departments are encouraged to report laboratory-confirmed cases to CDC through ArboNET, the national surveillance system for arboviral disease..
Treatment
No specific antiviral treatment is available for Zika virus disease. Treatment is generally supportive and can include rest, fluids, and use of analgesics and antipyretics. Because of similar geographic distribution and symptoms, patients with suspected Zika virus infections also should be evaluated and managed for possible dengue or chikungunya virus infection. Aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) should be avoided until dengue can be ruled out to reduce the risk of hemorrhage. People infected with Zika, chikungunya, or dengue virus should be protected from further mosquito exposure during the first few days of illness to prevent other mosquitoes from becoming infected and reduce the risk of local transmission.
Diagnostic Testing
During the first week after onset of symptoms, Zika virus disease can often be diagnosed by performing reverse transcriptase-polymerase chain reaction (RT-PCR) on serum. Virus-specific IgM and neutralizing antibodies typically develop toward the end of the first week of illness; cross-reaction with related flaviviruses (e.g., dengue and yellow fever viruses) is common and may be difficult to discern. Plaque-reduction neutralization testing can be performed to measure virus-specific neutralizing antibodies and discriminate between cross-reacting antibodies in primary flavivirus infections.
Zika virus (ZIKV) is a member of the Flaviviridae virus family and the Flavivirus genus.
In humans, it initially causes a mild illness known as Zika fever, Zika, or Zika disease, which since the 1950s has been known to occur within a narrow equatorial belt from Africa to Asia. In 2014, the virus spread eastward across the Pacific Ocean to French Polynesia, then to Easter Island and in 2015 to Central America, the Caribbean, and South America, where the Zika outbreak has reached pandemic levels.[1] Zika virus is related to dengue, yellow fever, Japanese encephalitis, and West Nile viruses.[2] The illness it causes is similar to a mild form of dengue fever,[2] is treated by rest,[3] and cannot be prevented by drugs or vaccines.[3]There is a possible link between Zika fever and microcephaly in newborn babies of infected mothers.[4][5][6]
In January 2016 the U.S. Centers for Disease Control and Prevention (CDC) issued travel guidance on affected countries, including the use of enhanced precautions and considering postponing travel, and guidelines for pregnant women.[7][8] Other governments or health agencies soon issued similar travel warnings,[9][10][11] while Colombia, theDominican Republic, Ecuador, El Salvador, and Jamaica advised women to postpone getting pregnant until more is known about the risks.[10][12]
| Zika virus | |
|---|---|
| Virus classification | |
| Group: | Group IV ((+)ssRNA) |
| Family: | Flaviviridae |
| Genus: | Flavivirus |
| Species: | Zika virus |
| Zika fever | |
|---|---|
| Classification and external resources | |
| Specialty | Infectious disease |
| ICD-10 | A92.8 |
Virology
Along with other viruses in this family, Zika virus is enveloped and icosahedral with a nonsegmented, single-stranded, positive-sense RNA genome. It is most closely related to the Spondweni virus and is one of the two viruses in the Spondweni virus clade.[13][14]
The virus was first isolated in 1947 from a rhesus macaque in the Zika Forest of Uganda and in 1968 was isolated for the first time from humans in Nigeria.[15] From 1951 through 1981, evidence of human infection was reported from other African countries such as the Central African Republic, Egypt, Gabon, Sierra Leone,Tanzania, and Uganda, as well as in parts of Asia including India, Indonesia, Malaysia, the Philippines, Thailand, and Vietnam.[15]
The pathogenesis of the virus is hypothesized to start with an infection of dendritic cells near the site of inoculation, followed by a spread to lymph nodes and the bloodstream.[13] Flaviviruses generally replicate in the cytoplasm, but Zika virus antigens have been found in infected cell nuclei.[16]
There are two lineages of Zika virus, the African lineage and the Asian lineage.[17] Phylogenetic studies indicate that the virus spreading in the Americas is most closely related to French Polynesian strains.[17] Complete genome sequences of Zika viruses have been published.[18] Recent preliminary findings from sequences in the public domain uncovered a possible change in nonstructural protein 1 codon usage that may increase the viral replication rate in humans.[19]
Transmission
Zika virus is transmitted by daytime-active mosquitoes and has been isolated from a number of species in the genus Aedes, such as A. aegypti, and arboreal mosquitoes such as A. africanus, A. apicoargenteus, A. furcifer, A. hensilli, A. luteocephalus, and A. vitattus. Studies show that the extrinsic incubation period in mosquitoes is about 10 days.[15] The vertebrate hosts of the virus are primarily monkeys and humans. Before the current pandemic, which began in 2007, Zika virus "rarely caused recognized 'spillover' infections in humans, even in highly enzootic areas".[20]
The potential societal risk of Zika virus can be delimited by the distribution of the mosquito species that transmit it (itsvectors). The global distribution of the most cited carrier of Zika virus, A. aegypti, is expanding due to global trade and travel.[21] A. aegypti distribution is now the most extensive ever recorded – across all continents including North America and even the European periphery.[22]
Recent news reports have drawn attention to the spread of Zika in Latin America and the Caribbean.[23] The countries and territories that have been identified by the Pan American Health Organisation (PAHO) as having experienced "local Zika virus transmission" are Barbados, Bolivia, Brazil, Colombia, the Dominican Republic, Ecuador, El Salvador, French Guiana, Guatemala, Guadeloupe, Guyana, Haiti, Honduras, Martinique, Mexico, Panama, Paraguay, Puerto Rico, Saint Martin, Suriname, and Venezuela.[24][25]
In 2009 Brian Foy, a biologist from the Colorado State University, sexually transmitted Zika virus to his wife. He visitedSenegal to study mosquitoes and was bitten on a number of occasions. A few days after returning to the United States, he fell ill with Zika, but not before having had unprotected intercourse with his wife. She subsequently showed symptoms of Zika infection with extreme sensitivity to light. Foy is the first person known to have passed on an insect-borne virus to another human by sexual contact.[26][27]
In 2015 Zika virus RNA was detected in the amniotic fluid of two fetuses, indicating that it had crossed the placenta and could cause a mother-to-child infection.[28]On 20 January 2016, scientists from the state of Paraná, Brazil, detected genetic material of Zika virus in the placenta of a woman who had undergone an abortion due to the fetus's microcephaly, which confirmed that the virus is able to pass the placenta.[29]
Clinical
Main article: Zika fever
Common symptoms of infection with the virus include mild headaches, maculopapular rash, fever, malaise, pink eye, and joint pains. The first well-documented case of Zika virus was described in 1964; it began with a mild headache, and progressed to a maculopapular rash, fever, and back pain. Within two days, the rash started fading, and within three days, the fever resolved and only the rash remained. Thus far, Zika fever has been a relatively mild disease of limited scope, with only one in five persons developing symptoms, with no fatalities, but its true potential as a viral agent of disease is unknown.[15]
As of 2016, no vaccine or preventative drug is available. Symptoms can be treated with paracetamol (acetaminophen), while aspirinand other nonsteroidal anti-inflammatory drugs should be used only when dengue has been ruled out to reduce the risk of bleeding.[30]
In a French Polynesian epidemic, 73 cases of Guillain–Barré syndrome and other neurologic conditions occurred in a population of 270,000, which may be complications of Zika virus.[20] In December 2015, the European Centre for Disease Prevention and Control issued a comprehensive update on the possible association of Zika virus with congenital microcephaly and this syndrome.[31]
Microcephaly
Data suggests that newborn babies of mothers who had a Zika virus infection during the first trimester of pregnancy are at an increased risk of microcephaly.[32] In December 2015 it was suspected that a transplacental infection of the fetus may lead to microcephaly and brain damage.[33][34] The Brazilian Ministry of Health has since confirmed the relation between the Zika virus and microcephaly.[4]
History
In 1947 scientists researching yellow fever placed a rhesus macaque in a cage in the Zika Forest (zika meaning "overgrown" in the Luganda language), near theEast African Virus Research Institute in Entebbe, Uganda. The monkey developed a fever, and researchers isolated from its serum a transmissible agent that was first described as Zika virus in 1952.[35] It was subsequently isolated from a human in Nigeria in 1954. From its discovery until 2007, confirmed cases of Zika virus infection from Africa and Southeast Asia were rare.[36]
In April 2007 the first outbreak outside of Africa and Asia occurred on the island of Yap in the Federated States of Micronesia, characterized by rash, conjunctivitis, and arthralgia, which was initially thought to be dengue, Chikungunya, or Ross River disease.[37] However, serum samples from patients in the acute phase of illness contained RNA of Zika virus. There were 49 confirmed cases, 59 unconfirmed cases, no hospitalizations, and no deaths.[38] More recently, epidemics have occurred in Polynesia, Easter Island, the Cook Islands, and New Caledonia.[36]
Since April 2015, a large, ongoing outbreak of Zika virus that began in Brazil has spread to much of South and Central America, and the Caribbean. In January 2016, the CDC issued a level 2 travel alert for people traveling to regions and certain countries where Zika virus transmission is ongoing.[39] The agency also suggested that women thinking about becoming pregnant should consult with their physicians before traveling.[40] Governments or health agencies of the United Kingdom,[9] Ireland,[10] New Zealand,[41] Canada,[11] and the European Union[11] soon issued similar travel warnings. In Colombia, Minister of Health and Social Protection Alejandro Gaviria Uribe recommended to avoid pregnancy for eight months, while the countries of Ecuador, El Salvador, and Jamaica have issued similar warnings.[10][12]
Plans were announced by the authorities in Rio de Janeiro, Brazil, to try to prevent the spread of the Zika virus during the 2016 Summer Olympic Games in that city.[11]
According to the CDC, Brazilian health authorities reported more than 3,500 microcephaly cases between October 2015 and January 2016. Some of the affected infants have had a severe type of microcephaly and some have died. The full spectrum of outcomes that might be associated with infection during pregnancy and the factors that might increase risk to the fetus are not yet fully understood. More studies are planned to learn more about the risks of Zika virus infection during pregnancy.[42] In the worst affected region of Brazil approximately 1 percent of newborns are suspected of microcephaly.[43]
Question and Answers: Zika virus infection (Zika) and pregnancy
Is there a vaccine to prevent or medicine to treat Zika?
No. There is no vaccine to prevent infection or medicine to treat Zika.
I am pregnant. Should I travel to a country where cases of Zika have been reported?
Until more is known, and out of an abundance of caution, CDC recommends special precautions for pregnant women and women trying to become pregnant:
- Pregnant women in any trimester should consider postponing travel to the areas where Zika virus transmission is ongoing. Pregnant women who do travel to one of these areas should talk to their doctor or other healthcare provider first and strictly follow steps to avoid mosquito bites during the trip.
- Women trying to become pregnant who are thinking about becoming pregnant should consult with their healthcare provider before traveling to these areas and strictly follow steps to prevent mosquito bites during the trip.
Because specific areas where Zika virus transmission is ongoing are difficult to determine and likely to change over time, CDC will update this travel notice as information becomes available. Check the CDC travel website frequently for the most up-to-date recommendations.
I am pregnant. How will Zika virus affect me or my unborn baby?
CDC has issued a travel notice (Level 2-Practice Enhanced Precautions) for people traveling to regions and certain countries where Zika virus transmission is ongoing.
This alert follows reports in Brazil of microcephaly and other poor pregnancy outcomes in babies of mothers who were infected with Zika virus while pregnant. However, additional studies are needed to further characterize this relationship. More studies are planned to learn more about the risks of Zika virus infection during pregnancy.
Until more is known, and out of an abundance of caution, CDC recommends special precautions for pregnant women and women trying to become pregnant:
- Pregnant women in any trimester should consider postponing travel to the areas where Zika virus transmission is ongoing. Pregnant women who do travel to one of these areas should talk to their doctor or other healthcare provider first and strictly follow steps to avoid mosquito bites during the trip.
- Women trying to become pregnant should consult with their healthcare provider before traveling to these areas and strictly follow steps to prevent mosquito bites during the trip.
Because specific areas where Zika virus transmission is ongoing are difficult to determine and likely to change over time, CDC will update this travel notice as information becomes available. Check CDCs Zika Travel Information website frequently for the most up-to-date recommendations.
Is it safe to use an insect repellent if I am pregnant or nursing?
Yes! Using an insect repellent is safe and effective. Pregnant women and women who are breastfeeding can and should choose an EPA-registered insect repellents and use it according to the product label.
If a woman who is not pregnant is bitten by a mosquito and infected with Zika virus, will her future pregnancies be at risk?
No. If infected Zika virus usually remains in the blood of an infected person for about a week. The virus will not cause infections in a baby that is conceived after the virus is cleared from the blood.
Should a pregnant woman who traveled to an area with Zika virus be tested for the virus?
See your healthcare provider if you are pregnant and develop a fever, rash, joint pain, or red eyes within 2 weeks after traveling to a country where Zika virus cases have been reported. Be sure to tell your health care provider where you traveled.
Can a previous Zika virus infection cause someone who later becomes pregnant to have an infant with microcephaly?
We do not know the risk to the baby if a woman is infected with Zika virus while she is pregnant. However, Zika virus infection does not pose a risk of birth defects for future pregnancies. Zika virus usually remains in the blood of an infected person for about a week. The virus will not cause infections in a baby that is conceived after the virus is cleared from the blood.
Is it safe to get pregnant after traveling to a country with Zika virus?
If infected, Zika virus usually remains in the blood of an infected person for about a week. The virus will not cause infections in a baby that is conceived after the virus is cleared from the blood.
Can a pregnant woman be tested for Zika weeks or months after being in a country with Zika?
At this time, and for several reasons, we do not recommend routine Zika virus testing in pregnant women who have traveled to a country with known transmission. First, there can be false-positive results due to antibodies that are made against other related viruses. Second, we do not know the risk to the fetus if the mother tests positive for Zika virus antibodies. We also do not know if the risk is different in mothers who do or do not have symptoms due to Zika virus infection.

The leader of infectious disease research in the U.S. government says that the pandemic of Zika virus spreading across the global south, which may be causing an epidemic of birth defects in South America, heralds a new kind of infectious disease threat. It is exploding at the same time and in the same areas as other diseases carried by the same vector, mosquitoes—and thus demonstrates that it is no longer enough to be prepared to counter one disease at a time.
Dr. Anthony Fauci, the director of the National Institute of Allergy and Infectious Diseases at the National Institutes of Health, writes in a study released Wednesday in the New England Journal of Medicine with Dr. David Morens of NIAID that Zika arrives in the Americas on the heels of three other mosquito-borne diseases: West Nile virus, in the United States since 1999 and still causing cases; chikungunya, which has invaded the Caribbean and Central America; and dengue, which moved north from the tropics to become re-established in Florida.
“Zika virus forces us to confront a potential new disease-emergence phenomenon: pandemic expansion of multiple, heretofore relatively unimportant arboviruses previously restricted to remote ecologic niches,” they write. “To respond, we urgently need research on these viruses and the ecologic, entomologic, and host determinants of viral maintenance and emergence. Also needed are better public health strategies to control arboviral spread.”
As I reported a month ago, Zika—which is often a mild disease of fever, aches and rash—has spiked extraordinary alarm in Brazil because it is overlaid with, and may be causing, an epidemic of babies being born with unusually small brains and heads. The microcephaly, as it is called, has not been proven to be caused by Zika, but people are so alarmed that, as one commenter here wrote, “People here are very worried about Zika virus, especially pregnant women and the ones trying to get pregnant… In the timespan of two weeks my city has gone from ‘never heard of this virus’ to thousands of infecteds, inclunding myself, my husband, and several relatives and friends of mine.”
At that point, Zika had spread from the shoulder of South America up through Central America and into Mexico. Since then, it has also been found in Puerto Rico, in a person who had not traveled outside the country—putting it on U.S. soil though not in the continental United States—and on Monday, in the vicinity of Houston, though that person was probably infected while traveling.
Zika, dengue and chikungunya are spread by the same mosquito species, A. aegypti, which has adapted to live near humans: It flourishes in small pools and containers of water, like a flower pot or the puddle in a tire. There are limited tests for the diseases—none for Zika, and sparsely distributed ones for the other two —and no treatments for them other than supportive care. Their initial symptoms are similar, but because they have different serious complications—birth defects for Zika, hemorrhagic fever for dengue, reactive arthritis for chikungunya—it is possible to make mistakes in the early stages that can make the late consequences worse.
The researchers argue that all of this adds up to a new responsibility to both prevent diseases, and also confront that prevention is a broader task than has previously been understood. In the case of these mosquito-borne diseases, a “one bug one drug” approach is inadequate, they say. What is needed: broad-spectrum drugs that can address whole classes of viruses, and vaccine “platforms” that can be adjusted as needed to prevent infection with whatever virus arrives on the scene. But more broadly, these diseases provide a lesson, of how rapidly and lethally emerging threats—possibly, multiple threats— will take us by surprise if we do not prepare.
“In our human-dominated world, urban crowding, constant international travel, and other human behaviors combined with human-caused microperturbations in ecologic balance can cause innumerable slumbering infectious agents to emerge unexpectedly,” they write. “We clearly need to up our game with broad and integrated research that expands understanding of the complex ecosystems in which agents of future pandemics are aggressively evolving.”
Sumber : Ragam ilmiah dari internet


Tidak ada komentar:
Posting Komentar